Canada’s commitment to the care of injured, disabled, and aging Veterans dates back to the First World War. As part of this commitment, Veterans Affairs Canada (VAC) supports the needs of Veterans who require facility-based care. Through the Long-term Care (LTC) Program and the Intermediate Care component of the Veterans Independence Program (VIP-IC) (here after collectively referred to as the “Program”) VAC provides financial support for Veterans who require care. This care is provided in provincially licensed regulated or operated health care facilities, most of which provide care to other provincial residents as well as Veterans, including in the following settings:
- facilities such as nursing homes and other long-term care facilities with beds that are open to Veterans as well as other provincial residents; and
- facilities with beds designated through contractual arrangements with the province, health authority and/or facility for priority access for World War II and Korean War Veterans.Footnote 1
The support that VAC provides for Veterans who need long-term care is laid out in the Veterans Health Care Regulations (VHCRs). Veteran eligibility for long-term care support, as well as the type of long-term care setting, depends on the type and location of military service, income, health care need, and whether or not the need for long-term care is related to a disability from military service.
1.1 Program Overview
Generally speaking, Second World War and Korean War Veterans can access a fixed number of contract beds designated in certain facilities across the country. Factors taken into consideration when determining eligibility include:
- health care need;
- service-related disability;
- income; and
- military service.
VAC contributes up to 100% of the cost of contract beds, depending on the Veteran’s eligibility and the facility they access. As of September 30, 2018, VAC had an allocation of 3,309 contract beds at over 156 facilities across Canada
All other Veterans, such as those who served with Allied armed forces Footnote 2, War Veterans who served in Canada only, and Canadian Armed Forces (CAF) Veterans who need care due to service-related disability or frailty Footnote 3 may be eligible for financial support for long-term care in community beds. Veterans can access these beds in the same manner as other Canadians and may be placed on a provincial waitlist. See Appendix A for program eligibility groups and group definitions.
As of March 31, 2018, VAC was supporting 5,110 Veterans in approximately 1,318 nursing homes and other long-term care facilities across Canada. Long-term care funding for 2,012 Veterans was issued through VIP-IC while 3,098 Veterans were funded through the LTC Program. Significantly more Veterans resided in community beds than contract beds (3,300 versus 1,810).
A breakdown of VAC expenditures and Program recipients for 2017-18 is detailed in Table 1 below:
| Care Setting | Recipients | Expenditures ($M) |
|---|---|---|
| Long-term Care (Contract Beds) | 1,810 | $175.6 |
| Long-term Care (Community Beds) | 1,288 | $16.8 |
| VIP-IC (Community Beds) | 2,012 | $44.6 |
| Totals | 5,110 | $237.0 |
Source: VAC Facts and Figures March 2018.
The number of CAF Veterans receiving support for long-term care is rising as the CAF cohort ages (as of March 2018, 32% of CAF Veterans receiving VAC benefits are over age 70 and 14% are over age 80). However, this is being more than offset by a declining war service long-term care population that is forecasted to decrease by 61% between 2019 and 2023.
As of March 2018, over 99% of war service Veterans receiving any VAC benefit or service were over the age of 80, with 86% being over the age of 90. As Figure 1 shows, by 2022-23 the total number of Veterans in receipt of long-term care benefits is forecasted to decline to approximately 2,900.
Figure 1 – Actual and Forecasted LTC and VIP IC Recipients 2014-23
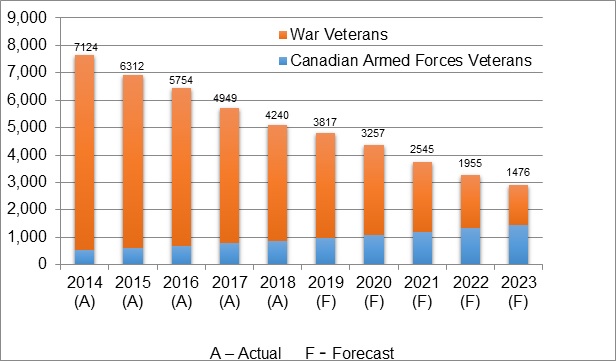
Source: VAC’s Statistics Directorate
Figure 1 – Actual and Forecasted LTC and VIP IC Recipients 2014-23
| Canadian Armed Forces Veterans | War Veterans | |
|---|---|---|
| 2014 (A) | 535 | 7124 |
| 2015 (A) | 597 | 6312 |
| 2016 (A) | 687 | 5754 |
| 2017 (A) | 781 | 4949 |
| 2018 (A) | 870 | 4240 |
| 2019 (F) | 989 | 3817 |
| 2020 (F) | 1098 | 3257 |
| 2021 (F) | 1207 | 2545 |
| 2022 (F) | 1324 | 1955 |
| 2023 (F) | 1441 | 1476 |
1.2 Long-term Care in Canada
Interviews with VAC staff and representatives from long-term care facilities indicate that a growing demand for beds is putting pressure on available resources and that provincial waitlists are growing. Research shows that the need for long-term care is rising. A 2017 Conference Board of Canada report on LTC projects a near doubling in the need for long-term care beds as the number of Canadians aged 75+ significantly increases. The report indicates that the 2016 national complement of 255,000 beds must be increased by 199,000 between 2017 and 2035 to meet demandFootnote 4. As Figure 1 above shows, VAC is forecasting an 85% increase in demand by CAF Veterans, which is similar to the increase the Conference Board of Canada is projecting for the broader Canadian population.
Long-term care waitlists in Ontario are a good example of how shifting demographics in Canada are placing high demands on provincial long-term care programs. As of April 2018, 32,835 residents in Ontario were waiting for placement in long-term care facilities, with an average wait time for admission of 158 days. This list has grown from 26,495 (24%) in 2015, despite increased investment in home care (i.e., aging in place strategies).Footnote 5 In some facilities, the wait time for admission far exceeds the average.
1.3 Program Eligibility and Funding
The delivery of long-term care in Canada is a provincial/territorial responsibility. Veterans are assessed by Provincial Health Authority staff and/or VAC nurses to determine if they need long-term care before receiving long-term care financial support.
To be eligible for long-term care financial support from VAC, a Veteran must:
- be assessed as needing long-term care by a health care professional; and
- meet service eligibility requirements.
Long-term care can be assessed through 29 eligibility gateways (when including frailty). See Appendix A for a listing of the eligibility gateways.
Since the Department first began transferring former Veterans hospitals from federal to provincial jurisdiction in the mid-1960s, various funding arrangements have been put in place depending on the province, the facility and bed type as well as the realities of the provincial health care systems at that time.Footnote 6 For example:
- in some instances, VAC pays for the full cost of care including facility operating costs;
- in some instances, VAC pays for the care of the Veteran, but not for additional facility operating costs; and
- in some provinces or facilities VAC only pays for enhanced programming for Veterans.
1.4 Preferred Admission Beds Initiative
Prior to June 2016, there was increased demand on the Department to broaden the eligibility to contract beds at former Veterans hospitals. The Department responded by working with provincial partners to reach agreements to re-profile beds that respected existing program eligibilities and allowed expedited access to a broader group of Veterans (including Allied Veterans, Canada Service Veterans and Canadian Armed Forces Veterans) at 18 former Veterans hospitals. This became known as the preferred admission beds initiative.Footnote 7
To date, short-term agreements have been signed with 10 of 18 former Veterans hospitals to re-profile contract beds to preferred admission beds (see Table 2). Negotiations continue with the remaining eight facilities. As Table 2 indicates, most preferred admission bed agreements were initially signed for a two-year period. This was intentional as the preferred admission beds initiative was designed as a short-term measure while the Department completed a review of its health care programs, including the Program’s eligibilities. The review, however, was not completed, necessitating the renewal of agreements at several facilities.
| Province | Facility | Contract Length | Initial Bed Allocation | Bed Allocation (as at September 30, 2018) | Number occupied (as at September 30, 2018) |
|---|---|---|---|---|---|
| Alberta | Carewest Colonel Belcher | 2 year | 10 | 10 | 10 |
| British Columbia | The Veterans Memorial Lodge at Broadmead | 2 year | 10 | 10 | 12* |
| New Brunswick | Ridgewood Veterans Wing | 2 year | 10 | 15 | 16* |
| New Brunswick | Veterans Health Unit | 2 year | 7 | 7 | 6 |
| Nova Scotia | Camp Hill Veterans Memorial BuildingFootnote 8 | 2 year | 15 | 25 | 25 |
| Ontario | Parkwood Institute | 2 year | 10 | 20 | 13 |
| Ontario | Perley and Rideau Veterans’ Health Centre | 2 year Pilot between the facility and the province of Ontario supported by VAC | 25 | 25 | 23 |
| Ontario | Sunnybrook Health Sciences Centre | 2 year | 30 | 50 | 54* |
| Quebec | Maison Paul-Triquet | 2 year | 15 | 15 | 13 |
| Saskatchewan | Wascana Extended Care/Veterans Program Footnote 9 | 1 year | 5 | 5 | 0 |
| Total | 137 | 182 | 172 |
Source: VAC’s Service Delivery and Program Management Division LTC Contract Bed Report September 30, 2018. Note that occupancy numbers are a snapshot in time and not an indication of demand. Open beds may be a result of natural turn-over duration (e.g. it may take several days for an empty room to be prepared). Also, Veterans could be waiting for a bed in a unit that is better able to meet his or her needs.