Identifying Risk Groups at Release
Simkus K, VanTil L. 2018 Veteran Suicide Mortality Study: Identifying Risk Groups at Release. Charlottetown (PE): Veterans Affairs Canada, Research Directorate Technical Report; 4 December, 2018
Executive Summary
Deaths by suicide in our Veteran population are tragic and a top public health concern. Veterans Affairs Canada (VAC) is committed to the well-being of its Veterans, and researching and preventing suicides is one of the department’s health priorities.
The Veteran Suicide Mortality Study (VSMS) uses Department of National Defence military career records of over 200,000 former Regular Force and Reserve Class C personnel linked to Canadian death records at Statistics Canada, and follows a cohort of Veterans who released from the Canadian Armed Forces (CAF) between 1976 and 2012. In 2017, the VSMS measured the magnitude of suicide in the CAF Veteran population. Both males and females were significantly more likely to die by suicide than the Canadian general population over the approximately four decades examined. Male Veterans were at highest risk of suicide in the youngest age groups, and the risk decreased with age. The suicide risk in female Veterans did not change with age.
Using the same data, the 2018 VSMS aimed to identify subpopulations within the Veteran community who were at higher risk of suicide, and also identify how many years after release Veterans were at greatest risk of dying by suicide. Cox proportional models, hazard ratios, age-adjusted rates, and standardised mortality ratios were used to identify risk factors at release from the CAF, in addition to changes in suicide risk over time after release.
The 2018 VSMS resulted in four key findings:
- For male Veterans, suicide risk was greatest in those who were Junior Non-Commissioned Members (NCM) at release and those who had a non-voluntary release. Suicide risk decreased as age at release increased. Veterans with Class C Reserve service had a similar risk of suicide as those with Regular Force service.
- Male Veteran suicide rates where highest in the first decade after release and decreased to Canadian male levels after 20 years. Males were at highest risk of suicide approximately four years after release.
- For female Veterans, suicide risk was greatest in those who were NCMs at release. Age at release, age at death, and component were not significantly associated with an increased risk of suicide.
- Female Veteran suicide rates were lowest in the first decade after release, highest in the second decade after release, then decreased to Canadian female levels after 20 years. Females were at highest risk of suicide approximately twenty years after release.
These findings provide evidence to implement suicide prevention interventions beyond the first few years after release from the CAF, and target prevention activities towards NCMs, Veterans who released at a young age, and non-voluntary releases. In addition, the differing trends between females and males in regards to suicide risk by age at death, age at release, and time since release provide strong evidence to ensure prevention and treatment efforts take into account their differing risk profiles.
Introduction
A Veteran’s suicide is tragic and has far-reaching impacts on the deceased’s family, friends, co-workers, and the communities to which they are connected. Veterans Affairs Canada (VAC) has established suicide surveillance and research as a public health priority, and is committed to monitoring and conducting further analysis on Veteran suicides to support ongoing suicide prevention activities.
The Veteran Suicide Mortality Study (VSMS) is a collaborative study between VAC, the Department of National Defence (DND), and Statistics Canada (STC). The aims of the VSMS are the following: to enhance the understanding of factors associated with suicide in CAF Veterans, to provide updates on suicide trends over time, to aid in the discussion of suicide prevention activities, and to respond to the ongoing public expectation for timely reporting.
After military personnel leave the Canadian Armed Forces (CAF), they receive health care from provincial and territorial health services, and their medical and mortality data are not routinely captured by VAC. To identify Veterans in the Canadian vital statistics databases, VAC and DND worked together to identify a cohort of over 200,000 released Regular Force and Reserve C Force (deployed) personnel from the DND administrative databases, which was then linked to death records at STC.
To identify risk factors for suicide associated with military service in serving and released CAF personnel, in 2011, VAC and DND conducted the Canadian Forces Cancer and Mortality Study (CF CAMS). Using a Cox proportional hazards model, the study found that male sex, young age, releasing as an NCM, and having a non-voluntary release were factors that all increased the risk of dying by suicide (STC, 2011).
In 2017, epidemiologists at VAC completed the analysis for the first VSMS using improved and more complete data sources from DND. The 2017 VSMS focused on quantifying the risk of suicide in the Veteran population compared to the Canadian General Population (CGP), and examined trends over time. Both male and female Veterans were found to have a higher risk of dying by suicide compared to their civilian counterparts, and the risk of suicide was relatively unchanged over the four decades studied.
Having established that the risk estimates for suicide remained stable over time, the full 37-year cohort could now be used to identify other characteristics of groups of Veterans at greatest suicide risk at release from the CAF, as well as identify what time periods after release Veterans were at greatest risk of suicide. Here, we examine military information available at time of release from the CAF, including component, rank, reason for release, age at release, and time since release.
Methods
The VSMS cohort included Regular Force and Class C Reservist Veterans who released from the CAF between 1976 and 2012. DND pay data and other administrative data were used to create a military occupational history for each Veteran (Appendices A and B). Analysts at STC linked these military data to death records from the provinces and territories, which include information on date and cause of death. The 37-year study follow-up period was defined by the earliest date (1976) that Veterans could be identified in the DND pay records, and the latest date (2012) that STC mortality data were available at the time of data linkage. Suicide deaths were identified in the death records by the World Health Organisation’s (WHO) International Classification of Diseases (ICD) codes (Appendix C). The 2018 VSMS uses the same cohort of Veterans as the 2017 VSMS, and further description of how the dataset was created is explained in detail in earlier publications (Simkus, VanTil and Pedlar, 2017; Rolland-Harris et al., In Press).
The 2018 VSMS compared Veterans who died by suicide to those who did not. Cox proportional hazards models were used to compare risk factors and suicide outcomes between Veterans, adjusting for all other variables. Cox regression generated hazard ratios (HR), which can be interpreted in terms of relative risk compared to a reference category. As an example, if females were the reference category, an HR of 2.0 for males would imply that the relative risk of death was twice as high among males as it was among females. Conversely, an HR of 0.5 for males would imply that males had a risk of death half that of females. An HR of 1.0 would indicate that both males and females had a similar risk. 95% confidence intervals (CI) were also calculated; HRs with CIs that overlapped 1.0 were considered to be not statistically significant. For each model, multivariate-adjusted HRs were calculated to control for the other variables.
While the Cox model provided HRs to estimate the impact of sex, age at release, component, rank, and reason for release on the risk of suicide, the calculations of these estimates incorporate time since release. As a result, there were no HRs for time since release. However, survival and hazard curves were produced to visually portray how time since release affects suicide risk.
Survival functions were generated to examine the risk of suicide over time since release. For this study, the survival functions visually portray the probability of not dying by suicide at each time point since release from the CAF. In summary, a flat survival curve that remains close to 100% suggests that the likelihood of dying by suicide is low. However, when the survival curve drops sharply towards 0, this means that the risk of suicide is high at that time period. For rare events like suicide, it would be expected that the survival curve would not drop considerably below 100% as most Veterans are expected to live full lives beyond 37 years after release. To protect privacy, survival functions were smoothed to eliminate steps and the possibility of calculating the frequency of suicides by date from the charts.
Smoothed hazard functions were also generated to represent the instantaneous risk of suicide at each time point since release. These curves show how the rate of suicide increases, decreases, or remains constant over time since release. In this study where a rare health event (suicide) is being examined over a long period of time, hazard functions are best to identify at what points in time suicide risk increases, and at what points suicide risk decreases. Smoothed hazard curves are truncated at either end of the study time because the smoothing process requires averaging values over a moving window of data, resulting in these end points having insufficient data to provide accurate estimates. As well, the right ends of the curves may be unstable due to the small numbers caused by no longer being in the study, i.e. due to death (any cause) or having been released for fewer than 37 years (censoring).
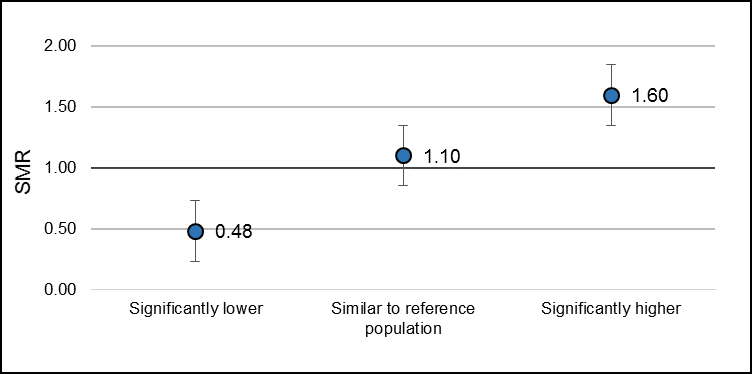
Standardised mortality ratios (SMR) were calculated for female Veterans to further investigate risk of suicide by age. SMRs were calculated using five-year age groups to compare the risk of suicide in Veterans to the CGP. A value of 1.0 suggests that the risk of death in the Veteran group is the same as the CGP. A value less than 1.0 suggests a lower risk, and a value greater than 1.0 suggests a higher risk. 95% CIs were also calculated; SMRs with CIs that overlapped 1.0 were considered to be not statistically significant.
To further examine time since release, age-adjusted suicide rates were calculated for Veterans by years since release from the CAF, using the suicide rates of the 2012 CGP as a comparison. Although most studies use the 1991 CGP as a reference population in Canada, it is becoming outdated. As a result, the most recent year available in the study (2012) was used to provide more up-to-date context to what is being observed in more recent years. 95% CIs were calculated to determine whether rates were statistically different from one another. The two methods in analysing time since release used two different references for comparison. The survival and hazard functions from the Cox model compared Veterans to other Veterans and control for component, rank, and age at release and reason for release. The age-adjusted rates compared Veteran suicide risk to the CGP, controlling only for age.
Last known military environment (Army, Air Force, and Navy) was not included in the analyses due to a significant amount (approximately 40%) of records not having any data on environment. Years of service were not included, since the year of enrollment was not available prior to 1976.
In compliance with STC privacy regulations, all risk factor categories, SMRs and rates were collapsed and presented in age groups or time period categories that ensured minimum cell counts of 10.
More detailed explanations of these methods are described in Appendix D.
Results
Cohort description
Starting with 9,885 Veterans who released in 1976, the VSMS cohort increased to 200,734 Canadian Veterans by the end of the study period in 2012 (Appendix A, Figure A-1) (Simkus, VanTil and Pedlar, 2017). The Veteran cohort was 89% male, 60% released at a Junior NCM rank, and 26% released since 2000. Some cohort members had a combination of service experience in both the Regular Force and as Class C Reservists during their careers. The majority of the cohort (95%) had been part of the Regular Force at some time in their military careers, and 14% had at least some Class C Reserve service time. See Appendix E for a more detailed description of the distribution of age and sex in the VSMS cohort.
Comparing suicide risk between male and female Veterans
Two Cox proportional hazard models were built to examine the risk of suicide between sexes; one controlling for component, rank, and age at release, and a second also controlling for reason for release and examining only the 1992 to 2012 portion of the cohort (Appendix F) (see Male Veterans 1992-2012 and reason for release subheading for more explanation).
For the full 1976 to 2012 cohort, compared to females, males had an HR of 2.82, and for the partial 1992 to 2012 cohort model which also controlled for reason for release, males had an HR of 3.86. Both these HRs were statistically significant. However, the models violated the proportional-hazards assumption (p=0.0021 and 0.0428, respectively), indicating that the model should be built separately for males and females to examine the other risk factors. From this point on in the study, all analyses were completed separately for males and females.
Male Veterans 1976-2012
To examine suicide risk in male Veterans for the full 1976 to 2012 study period, a Cox model was built controlling for component (any Regular Force (RegF) service time vs. only Reserve Class C (ResC) service time), rank, and age at release. HRs and p-values generated from the multivariable regressions are presented in Table 1.
| Variable | Multivariable-adjusted hazard ratios (95% CI) | |
|---|---|---|
| Component | Any RegF service | Reference |
| Only ResC service | 0.95 (0.76-1.18) | |
| Rank at release | Junior NCM | 1.90 (1.56-2.31)* |
| Senior NCM | 1.32 (0.98-1.77) | |
| Junior Officer | Reference | |
| Senior Officer | 0.91 (0.55-1.51) | |
| Age at release | <25 | 2.82 (2.17-3.67)* |
| 25-34 | 2.13 (1.61-2.81)* | |
| 35-44 | 1.45 (1.12-1.87)* | |
| 45+ | Reference |
* HR is significantly different than 1.
1 No violations of proportionality assumption and model fit data well (Appendix H).
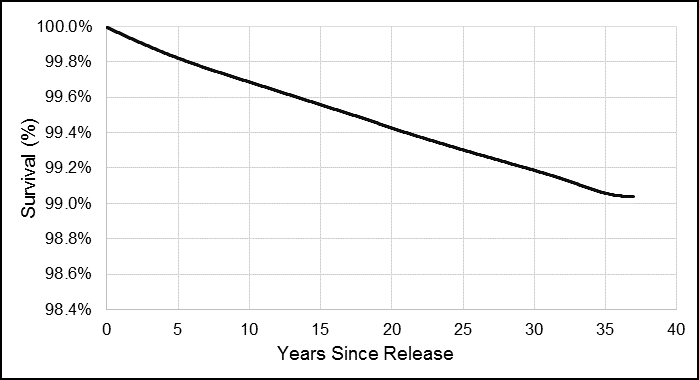
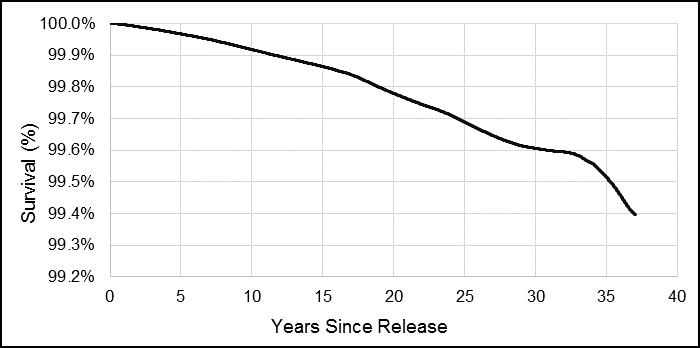
Overall, the risk of suicide, controlling for all other factors, remained generally constant, as demonstrated by an overall straight survival function curve (Figure 1). Over the 37-years of data, less than 1% of male Veterans in the cohort died by suicide, and therefore suicide remained a relatively rare event. Because this general trend was observed in all the male survival functions in this study, and since more information on risk over time can be garnered from the smoothed hazard functions, all other survival function graphs are presented together in Appendix G.
Figure 1. Male Veteran smoothed survival function for risk of dying by suicide, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
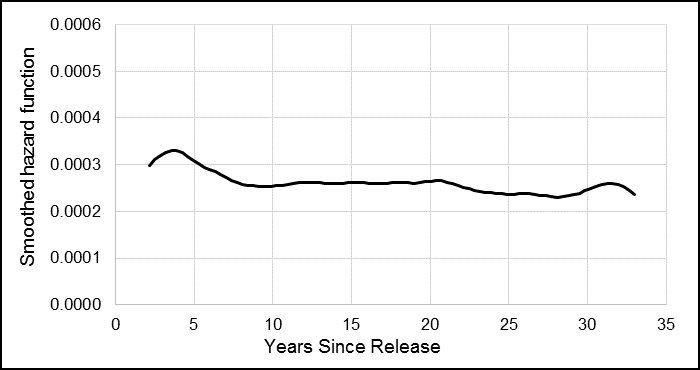
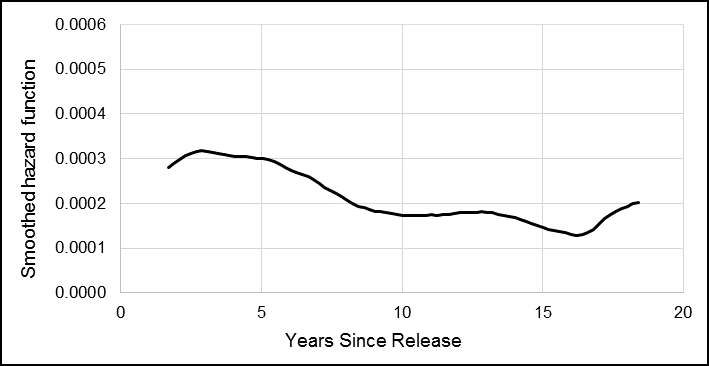
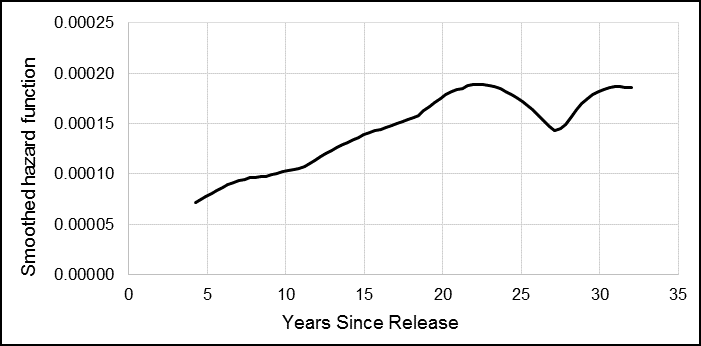
The smoothed hazard function curve showed the change in risk over time, and how for male Veterans, the risk of suicide was the highest approximately four years after release, and then decreased slightly or remained constant over the next three decades (Figure 2).
Figure 2. Male Veteran smoothed hazard function for risk of dying by suicide, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
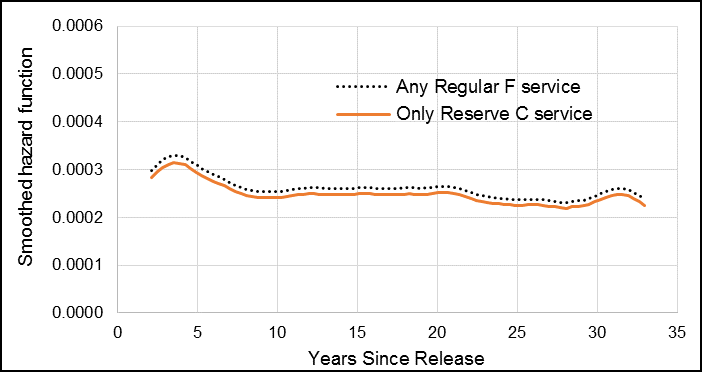
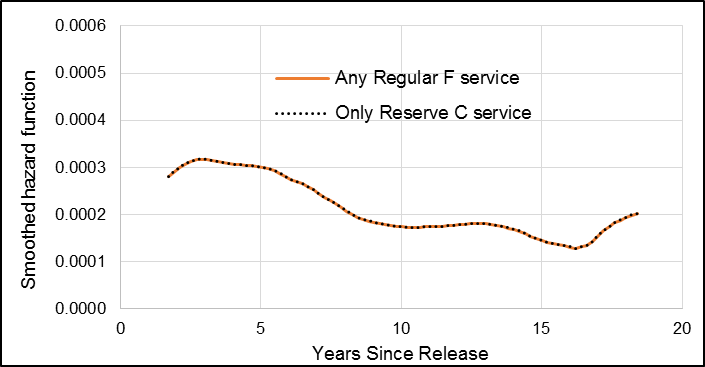
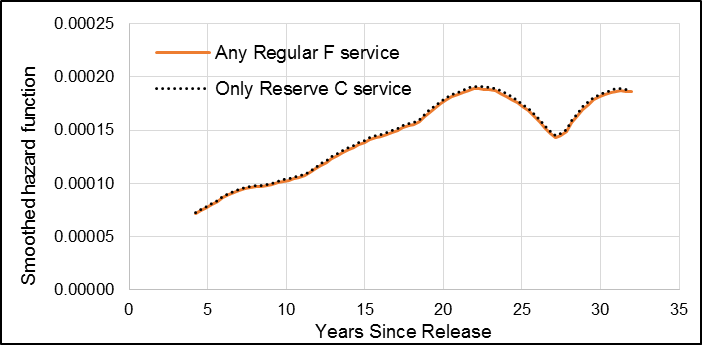
Adjusting for all other variables, male Veterans who had only reservist service time had a slightly lower risk of suicide than those with at least some Regular Force service time, but this was not statistically significant (Table 1). The hazard curve demonstrated visually how the suicide risk for the two component categories was similar (Figure 3).
Figure 3. Male Veteran smoothed hazard function for risk of dying by suicide by component (Regular Force vs. Reserve Force Class C service only), 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
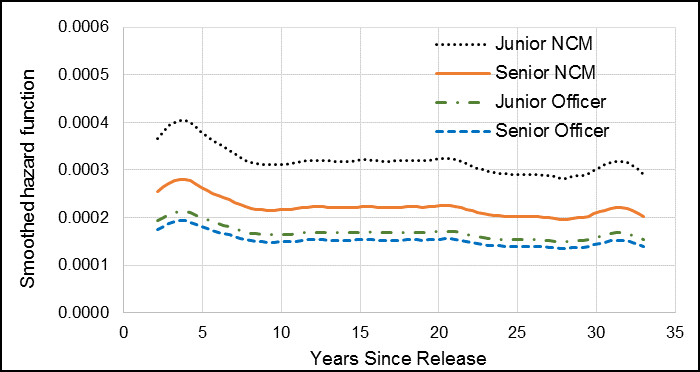
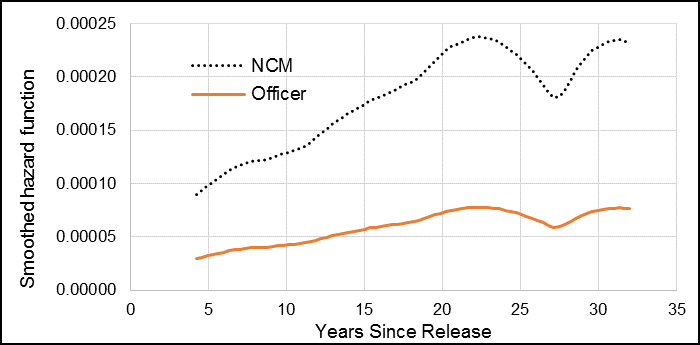
Compared to Veterans who released as Junior Officers (reference category), Junior NCMs had an HR of 1.90 and this was statistically significant (Table 1). Senior NCMs had an HR of 1.32, and Senior Officers had an HR of 0.91, but these were not statistically significant. This trend was observed in the hazard function curves for Junior Officers and Senior Officers, which were similar (Figure 4). The curves for Senior NCMs showed a greater hazard than Junior Officers over the study follow-up time, although this difference was not significantly different. Junior NCMs, however, had the greatest suicide hazard rate compared to the other ranks. In addition, the hazard curves for Officers had smaller fluctuations over time since release, while the hazard curve for Junior NCMs had a greater change in hazard in the first 10 years since release.
Figure 4. Male Veteran smoothed hazard function for risk of dying by suicide by rank at release, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
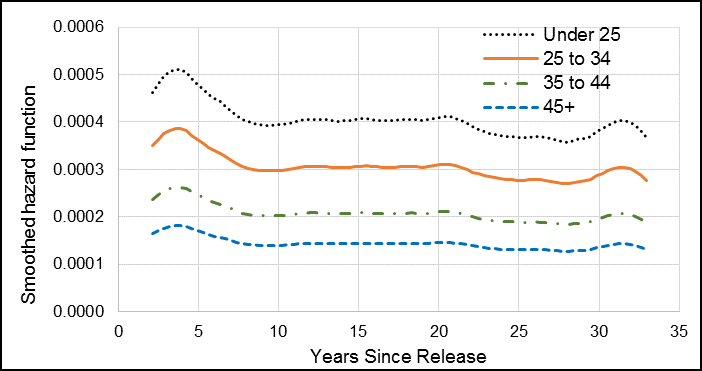
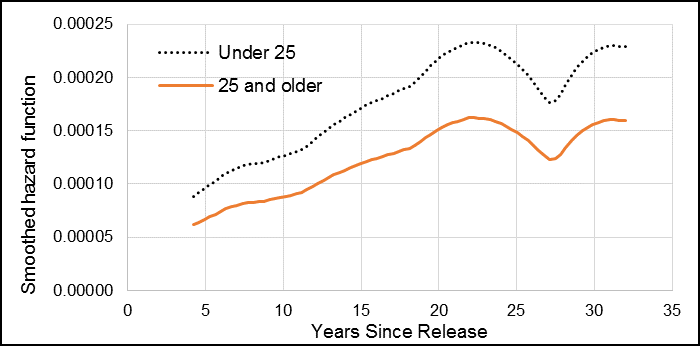
The risk of suicide decreased as age at release increased, with Veterans who released at age 24 and younger having an HR of 2.82 compared to those who released at age 45 or older (reference group) (Table 1). The risk of suicide was also elevated for those Veterans aged 25 to 34 (HR: 2.13) and 35 to 44 (HR: 1.45) at release, and these were all statistically significant. This trend was also observed in in the hazard functions, with male Veterans who released under age 25 being at greatest risk of suicide (Figure 5). The hazard function showed that Veterans who were younger when they released experienced a larger increase in suicide risk in the first few years after release, compared to Veterans who were older at release.
Figure 5. Male Veteran smoothed hazard function for risk of dying by suicide by age at release, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Male Veterans 1992-2012 and reason for release
A separate Cox model was built to examine reason for release. Analysis of temporal release trends revealed that the classification of reason for release between involuntary and medical changed significantly over the study period. Around 1992, there was a decrease in the proportion of CAF releases classified as involuntary, and an increase in the proportion of releases classified as medical (data not shown). The reason for this remains unknown at this time. As a result, only Veterans who released between 1992 and 2012 were examined to determine the risk of suicide by reason for release (Table 2).
| Variable | Multivariable-adjusted hazard ratios (95% CI) | |
|---|---|---|
| Component | Any RegF service | Reference |
| Only ResC service | 1.00 (0.53-1.89) | |
| Rank at release | Junior NCM | 1.53 (1.05-2.23)* |
| Senior NCM | 1.36 (0.86-2.16) | |
| Officer | Reference | |
| Age at release | <25 | 2.50 (1.51-4.15)* |
| 25-34 | 2.51 (1.56-4.04)* | |
| 35-44 | 1.94 (1.26-2.99)* | |
| 45+ | Reference | |
| Reason for release | Voluntary | Reference |
| Involuntary | 2.03 (1.46-2.83)* | |
| Medical | 1.72 (1.24-2.37)* |
* HR is significantly different than 1.
1 No violations of proportionality assumption and model fit data well (Appendix H).
Overall, the risk of suicide, controlling for all other factors, remained generally constant, although the effect of time since release on suicide risk was greater in the partial cohort than the full 1976 to 2012 cohort, as indicated by the slight curvatures in the survival curve (Figure 6).
Figure 6. Male Veteran smoothed survival function for risk of dying by suicide, 1992 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
The smoothed hazard curve showed that for male Veterans, the risk of suicide was greatest in the first approximately five years after release from the CAF, and then overall decreased over the next two decades (Figure 7). The apparent increase of suicide risk after approximately 16 years is likely due to small numbers and should be interpreted with caution.
Figure 7. Male Veteran smoothed hazard function for risk of dying by suicide, 1992 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
When examining the partial 1992 to 2012 cohort of male Veterans, male Veterans who had only reservist service time had the same risk of suicide as those with Regular Force time (HR: 1.00) (Table 2). The smoothed hazard curves demonstrated visually how there was no difference in suicide risk between the two component categories as the two curves overlapped (Figure 8).
Figure 8. Male Veteran smoothed hazard function for risk of dying by suicide by suicide by component (Regular Force vs. Reserve Force Class C service only), 1992 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Compared to Veterans who released as Officers (Junior and Senior combined), Junior NCMs had an HR of 1.53, and this was statistically significant (Table 2). Senior NCMs had an HR of 1.36, but this was not statistically significant. Similar to the full 1976 to 2012 cohort, Junior NCMs had the greatest change in hazard compared to the other ranks (Figure 9).
Figure 9. Male Veteran smoothed hazard function for risk of dying by suicide by suicide by rank at release, 1992 to 2012 releases.
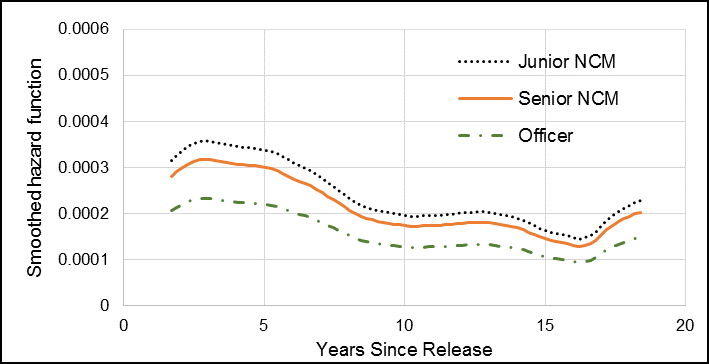
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Similar to the model using the full 1976 to 2012 cohort, the risk of suicide decreased as age at release increased, with Veterans who released at age 24 and younger having a statistically significant HR of 2.50 compared to those who released at age 45 or older (Table 2). This was almost identical to Veterans who released at age 25 to 34 (HR: 2.51). Those who released at 35 to 44 had an HR of 1.94, which was also statistically significant. The hazard functions showed that male Veterans who released under age 25 and between 25 and 34 years of age were at similar and the greatest risk of suicide (Figure 10). In addition, Veterans under 35 years at release experienced the largest increase in suicide risk in the first five years after release, while the suicide risk remained lower overall in Veterans who released at age 45 and older.
Figure 10. Male Veteran smoothed hazard function for risk of dying by suicide by suicide by age at release, 1992 to 2012 releases.
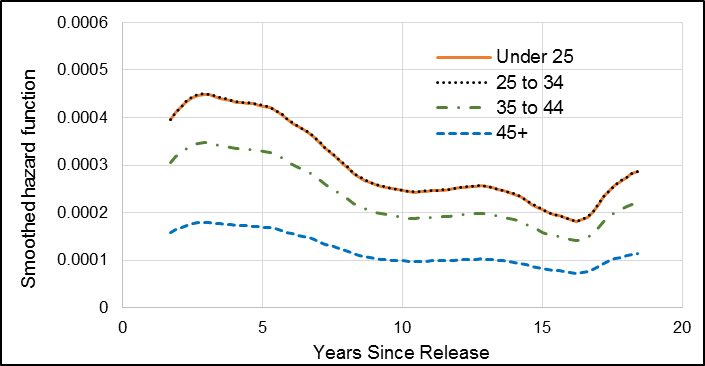
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
With the addition of reason for release to the Cox model, male Veterans who had an involuntary release between 1992 and 2012 had a statistically significant HR of 2.03 compared to those with a voluntary release (Table 2). Male Veterans who had a medical release had an HR of 1.72 compared to those who released voluntarily, and this was also statistically significant. The effect of reason for release was observed in the hazard function, where both those male Veterans who released involuntarily and medically had the greatest suicide risk (Figure 11). This difference was most notable within the first five years after release, after which it decreased quickly.
Figure 11. Male Veteran smoothed hazard function for risk of dying by suicide by suicide by reason for release, 1992 to 2012 releases.
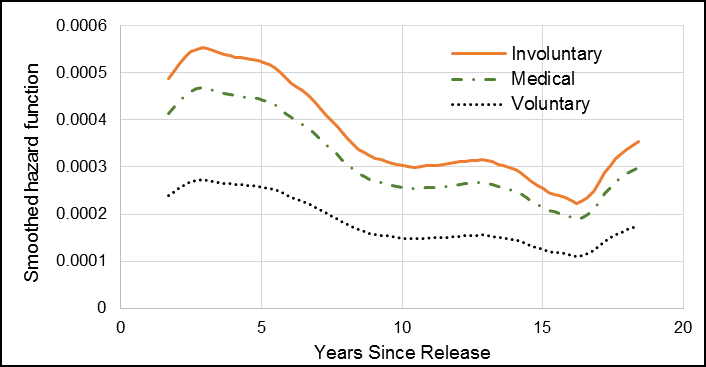
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Female Veterans 1976-2012
To examine suicide in female Veterans for the full 1976 to 2012 study period, a Cox model was built controlling for component, rank, and age at release (Table 3). Reason for release could not be included in the model due to small numbers in the non-voluntary release categories.
| Variable | Multivariable-adjusted hazard ratios (95% CI) | |
|---|---|---|
| Component | Any RegF service | Reference |
| Only ResC service | 1.01 (0.46-2.23) | |
| Rank at release | NCM | 3.05 (1.10-8.46)* |
| Officer | Reference | |
| Age at release | <25 | 1.44 (0.82-2.50) |
| 25+ | Reference |
* HR is significantly different than 1.
1 No violations of proportionality assumption and model fit data well (Appendix H).
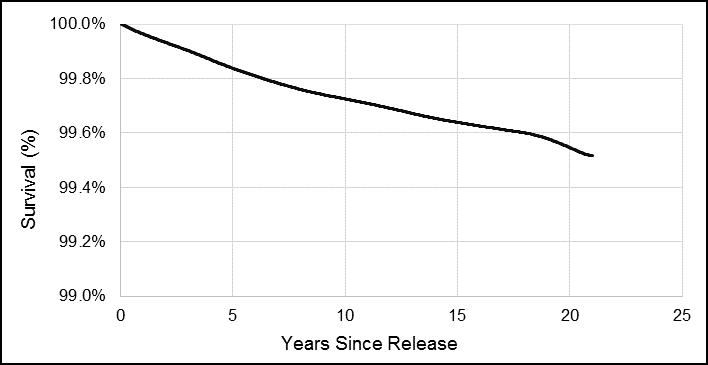
Overall, controlling for all other factors, the risk of suicide in female Veterans increased with time since release from the CAF (Figures 12 and 13). This is the opposite from what was seen in the male Veteran population. The survival function demonstrated how over the 37-years of data, approximately 0.6% of female Veterans in the cohort died by suicide, and therefore suicide remained a relatively rare event (Figure 12). Because this trend was observed in all of the female survival functions in this study, and more information on risk over time can be garnered from the smoothed hazard functions, all other survival functions are presented in Appendix G.
Figure 12. Female Veteran smoothed survival function for risk of dying by suicide, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
The smoothed hazard curve showed that for female Veterans, the risk of suicide increased relatively steadily over the first 20 years after release (Figure 13). Beyond 20 years, the trend should be interpreted with caution due to small numbers. For the purpose of these analyses, the risk of suicide is considered elevated after 20 years after release.
Figure 13. Female Veteran smoothed hazard function for risk of dying by suicide, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Adjusting for all other variables, female Veterans who had only Reserve Class C service had the same risk of suicide as those who had Regular Force service (HR: 1.01) (Table 3). This was also observed in the hazard curves as both curves for Regular Force and Reserve C service overlapped nearly completely (Figure 14).
Figure 14. Female Veteran smoothed hazard function for risk of dying by suicide by component (Regular Force vs. Reserve Force Class C service only), 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Compared to Veterans who released as Officers, NCMs (Junior and Senior combined) had a statistically significantly HR of 3.05 (Table 3). NCMs had a greater hazard compared to Officers (Figure 15). While the risk of suicide in female Officers increased only marginally over time, the risk of suicide in NCMs increased more steeply.
Figure 15. Female Veteran smoothed hazard function for risk of dying by suicide by rank at release, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Female Veterans who were under 25 years of age at release were at greater risk of suicide than those who released at age 25 years and older (HR: 1.44), but this was not statistically significant (Table 3). Although the hazard curve for female Veterans under 25 appeared to indicate that the risk of suicide was greater than in the older age group, this difference was not statistically significant (Figure 16).
Figure 16. Female Veteran smoothed hazard function for risk of dying by suicide by age at release, 1976 to 2012 releases.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Further examination of age at death in females
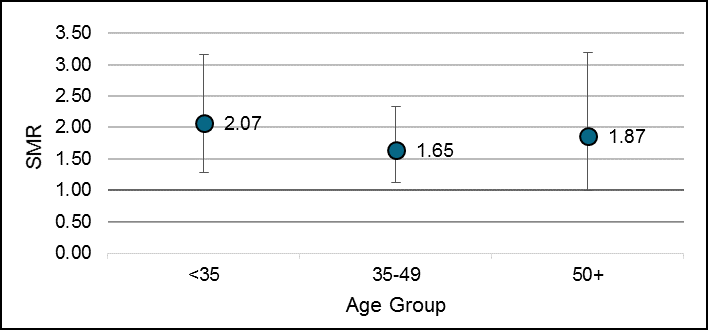
In the 2017 VSMS, SMRs were calculated to examine risk of suicide by age, sex, and over time. Due to small numbers, female Veterans were examined by only two age groups: under 45 years and 45 years and older. Both age groups had a statistically similar risk of dying by suicide. Here, further analyses were conducted to determine if this trend remained consistent if female Veterans were broken down into three age groups.
The risk of suicide remained elevated compared to the female CGP for female Veterans under 35 years (SMR: 2.07; 95% CI: 1.28, 3.16) and aged 35 to 49 (SMR: 1.65; 95% CI: 1.12, 2.34). Female Veterans aged 50 years and older were at a 1.87 times higher risk of dying by suicide compared to the female CGP, although this was not statistically significant (95% CI: 1.00, 3.20). However, overall, the risk of suicide in female Veterans did not differ significantly between the three age groups observed, with the confidence intervals for all three age groups overlapping (Table 4, Figure 17).
| Age group | Suicide SMR (95% CI) |
|---|---|
| Under 35 | 2.07 (1.28 - 3.16) |
| 35 to 49 | 1.65 (1.12 - 2.34) |
| 50 + | 1.87 (1.00 - 3.20) |
| Total | 1.81 (1.40 - 2.31) |
Figure 17. Comparison of female Veteran and female CGP suicide risks using SMRs by age group, 1976 to 2012.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
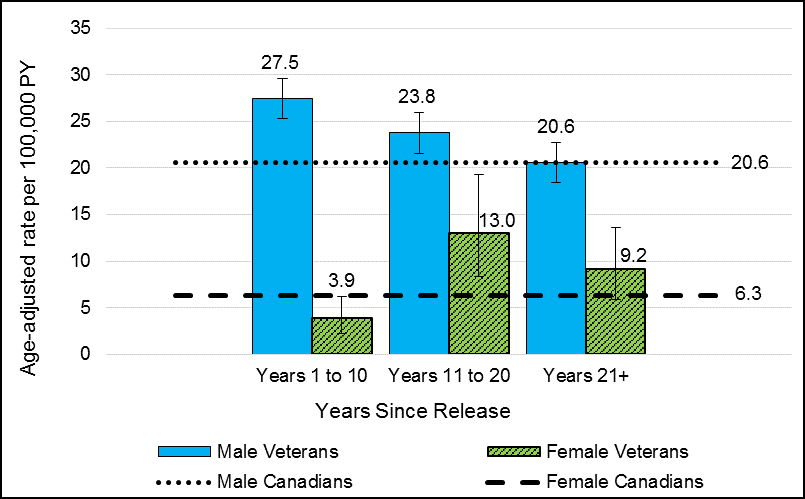
Male and female suicide rates
Age-adjusted rates for male and female Veterans were calculated by years since release from the CAF using the 2012 male and female CGPs as a reference (Figure 18). The age-adjusted suicide rate for male Veterans was highest in the first 10 years after release, and decreased to male CGP levels by the third decade after release. However, in contrast, female Veterans had the lowest rate of suicide during the first 10 years after release from the CAF, which was also significantly lower than the female CGP. However, the rate increased and was significantly higher than the CGP during years 11 to 20 after release. Over twenty years after release, female Veterans’ suicide rate decreased and not was statistically different from the CGP.
Figure 18. Age-adjusted suicide rates per 100,000 person-years (PY) in Veterans by sex and years since release, compared to the CGPs.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Discussion
Deaths by suicide in our Veteran population are tragic and a top public health concern. VAC continues to conduct research to understand why these deaths occur so that preventative actions can be taken. While the 2017 VSMS found that both male and female Veterans were at a significantly higher risk of suicide than the general population, further analyses were conducted in 2018 to identify potential risk factors at release. The key findings from this 2018 study are as follows:
- For male Veterans, suicide risk was greatest in those who were Junior NCMs at release and those who had a non-voluntary release. Suicide risk decreased as age at release increased. Veterans with Class C Reserve service had a similar risk of suicide as those with Regular Force service.
- Male Veteran suicide rates where highest in the first decade after release and decreased to Canadian male levels after 20 years. Males were at highest risk of suicide approximately four years after release.
- For female Veterans, suicide risk was greatest in those who were NCMs at release. Age at release, age at death, and component were not significantly associated with an increased risk of suicide.
- Female Veteran suicide rates were lowest in the first decade after release, highest in the second decade after release, then decreased to Canadian female levels after 20 years. Females were at highest risk of suicide approximately twenty years after release.
Here, these findings are discussed in further detail.
Comparing males and females
Just as suicidal behaviour differs between sexes, we expect to see differences in suicide risk between males and females in our Veteran population. Canadian males have a three to 3.5 times higher rate of suicide than Canadian females (Public Health Agency of Canada (PHAC), 2016; Navaneelan, 2016), and the 2017 VSMS found that when adjusted for age, the male to female age-adjusted suicide rate ratio for Veterans was also 3.5 (Simkus, VanTil and Pedlar, 2017; VanTil, Simkus and Rolland-Harris, 2018).
There were two estimates for suicide risk difference between male and female Veterans, with one model estimating that males were 2.8 times more likely, and the second estimating that males were 3.9 times more likely to die by suicide than females. Although these two estimates appear to be different, their confidence intervals both overlapped the 3.5 estimated suicide risk ratio from the 2017 VSMS, as well as the Canadian estimated male to female ratios. As a result, the difference in suicide risk between male to female Veterans is similar to the difference seen in the Canadian population, even when controlling for other military factors.
Although Veteran males were significantly more likely to die by suicide, previous research has shown that female Veterans had higher rates of suicide ideation and mental health disorders (MacLean et al., 2018). Higher rates of mental health disorders among females compared to males were also observed in serving CAF personnel (Pearson, Zamorski, and Janz, 2014). The contrasting trends between mental health prevalence and suicide risk between the sexes reinforce that the causes of suicide are multifactorial and not a result of mental health struggles alone (Thompson et al., Submitted; PHAC, 2016).
No study was identified in the literature that examined the risk of suicide by component, rank, or age at release in females specifically. Because most other studies combined both sexes into the analyses, it is unclear whether any female-specific trend has been diluted by the predominately male military populations. As a result, studies combining both sexes were used to compare to male CAF Veterans, but not females. In addition, to the best of our knowledge, this study is the first time the risk of suicide by years since release has been published for female Veterans.
Males by component
Veterans with Reserve Class C service had a similar risk of suicide as Regular Force Veterans. These findings support the analysis of both components together in future VSMS studies. This is consistent with previous research that found Veterans with both Reserve and Regular Force service time had health outcomes more similar to Regular Force Veterans than Reserve Force Veterans (VanTil et al., 2016).
The 2018 VSMS findings on component are consistent with other data linkage studies of suicide mortality, although they combine males and females. In Australia, suicide rates over the period of 2001 to 2015 were statistically similar for Regular and Reserve personnel in the cohort of serving personnel (Australian Institute of Health and Welfare (AIHW), 2017). In the United States (US), suicide rates over the period 2001 to 2009 were statistically similar for Regular and Reserve personnel in the cohort of serving and released military personnel (Reger et al., 2015).
Males by rank
Male Veterans who released as Junior NCMs were at highest risk of suicide. In the full 1976 to 2012 cohort, Junior NCMs were twice as likely to die by suicide as Junior Officers. Male Veterans who released as Senior NCMs were at a slightly higher risk of suicide than Officers, but this was not statistically significant.
We were unable to examine years of service as a risk factor; however, in general, Veterans who release at senior ranks are expected to have had longer service time than Veterans who release at junior ranks. Results from both the 2018 and 2017 VSMS suggest that younger age is strongly associated with an increased risk of suicide in male Veterans. However, even when controlling for age at release, Junior NCMs had a greater risk of suicide than Junior Officers, despite the similar length of service and level of seniority. Both Junior and Senior Officers had a statistically similar risk of suicide, despite Senior Officers having more years of service.
These findings suggest that rank (NCM vs. Officer) may be a more important predictor of suicide than length of service and possibly age. There may be characteristics observed in Junior NCMs that put them at greater risk of suicide than their Junior Officer counterparts, such as poorer mental health. Suicidal ideation was the highest in Veterans who released as Junior NCMs, and the prevalence of mental health conditions were higher in those who released as NCMs compared to Officers (VanTil et al., 2017). This same trend is observed at enrollment in the CAF; among CAF recruits, NCM candidates had a higher prevalence of mental disorders thanOfficer candidates, including depression, anxiety disorders, and PTSD (Lee and Hachey, 2011). Junior NCMs deployed to Afghanistan were significantly more likely to have mental disorders attributed to the mission than Officers, and a similar risk as Senior NCMs; however, rank did not have a significant effect on suicidal ideation (Boulos and Zamorski, 2016a). This suggests that NCMs are at higher risk of suicide at CAF enrollment, during service, and after their military careers.
The 2018 VSMS findings on rank are consistent with other data linkage studies of suicide mortality, although they combine males and females. In both Australia and the United Kingdom (UK), officers had half the risk of suicide compared to other ranks (AIHW, 2017; Kapur et al., 2009). In the US, suicide rates demonstrated a gradient from lowest rates for officer, higher rates for senior NCM (enlisted), and highest rates for junior NCM (enlisted) ranks (Reger et al., 2015).
Males by age at release
In male Veterans, the risk of dying by suicide decreased as age at release increased. Those who were under 25 at release were approximately three times more likely to die by suicide compared to males who released at 45 years and older. In addition, those who were aged 25 to 34 were approximately twice as likely, and those who were aged 35 to 44 at release were approximately 50 per cent more likely to die by suicide.
This same trend has been observed elsewhere. The earlier CF CAMS study of Veterans who enrolled and released between 1972 and 2006 found that for both males and females Veterans combined, the risk of suicide decreased with age at release, and that the risk of suicide was significantly higher in those who released under age 25 compared to those who released at age 25 or older (STC, 2011). Most other international studies examined age as a risk factor, but did not appear to specifically examine age at release. One UK Armed Forces Veteran study, however, found that for both males and females combined, the risk of suicide decreased with age, and was significantly higher for those who released under age 25 compared to those who released at age 45 to 59 (Kapur et al., 2009).
Males by reason for release
Male Veterans who had a non-voluntary release between 1992 and 2012 were approximately twice as likely to die by suicide as those who had a voluntary release.
This aligns with research of CAF Veterans where mental health, and to a lesser extent, physical health, were found to be associated with suicidal ideation (Thompson et al., 2014). Among Veterans who enrolled and released between 1972 and 2006, the risk of suicide (male and female combined) was significantly higher in those who had an involuntary release (HR: 1.55) or a medical release (HR: 2.03) than those who released voluntarily (STC, 2011). However, this study did not account for the changes in release classification over the study period, which were observed during the analysis for the 2018 VSMS.
Research from other countries often had similar findings. In Australia, male Veterans who were discharged involuntarily had a 2.4 times higher rate of suicide than those who discharged for voluntary reasons, and it was particularly higher in those who discharged for medical reasons (3.6 times the rate of those who released voluntarily) (AIHW, 2017). A study examining US military personnel found that compared to those with an honourable release, the risk of suicide was highest for those who did not have an honourable release (HR: 1.21), although a large portion of those studied had an unknown release characterisation (Reger et al., 2015). In contrast, a UK study found that there was no statistically significant difference in suicide risk between Veterans who had medical releases and those who had non-medical releases (Kapur et al., 2009).
Males by time since release
Overall, the risk of suicide peaked in male Veterans within the first decade after release, and this risk decreased with time. When comparing amongst Veterans and when controlling for other military factors, male Veterans had the greatest risk of suicide at approximately four years after release. When comparing to the male general population, male Veterans had the highest rate of suicide in the first decade after release. The peak in suicide risk immediately after release was not pronounced, and decreased until approximately 20 years after release when they reached Canadian male levels.
The overall decreasing trend of suicide risk with time since release aligned with findings from other countries. In Australia, the rate of suicide was highest in those males who had been released for less than six years, compared to those who been released six to 12 years; however, this difference was not found to be statistically significant (AIHW, 2017). A study of UK Armed Forces Veteran found the risk of suicide was persistent but may have been at highest in the first two years following release (Kapur et al., 2009). Lastly, a study examining US military personnel found that the risk of suicide was highest in the first year after release (HR: 2.64), and it gradually decreased with time (HR: 1.63 at 6 years or more since release) (Shen, Cunha, and Williams, 2016).
Females by component
Like males, female Veterans’ risk of suicide did not differ significantly by component. Suicide in female Veterans has not been examined specifically by component before, but these findings support recommendations to analyse female Veterans of Reserve Class C and Regular Force together.
Females by rank
For female Veterans, rank at release was the only risk factor in the Cox model that was highly and statistically significantly associated with suicide. Female Veterans who released as NCMs were over three times more likely to die by suicide than those who released as Officers. As discussed above with male Veterans, these findings suggest that there may be some characteristics unique to NCMs that put them at greater risk of suicide. While the difference in suicide risk between NCMs and Officers appears to be more pronounced in female Veterans than male Veterans, the confidence interval for this estimate is large (1.10 to 8.46) and therefore was not considered statistically different from what was observed in males.
Females by age at release
Females who released at under 25 years of age were 1.4 times more likely to die by suicide than those who released at age 25 years or older, but this was not statistically significant. This aligns with what was observed in the 2017 VSMS where age was not statistically significantly associated with risk of suicide in female Veterans. Unfortunately, due to small numbers, age at release cannot be examined in further detail other than under 25 vs. 25 years and older at release. This, in combination with the previous finding that NCMs had a significantly higher risk of suicide than Officers, controlling for age at release, adds to the evidence that NCM rank is a greater risk factor for suicide than years of service or seniority in the CAF.
Females by age at death
Females under 35 were at an approximately 2.0 times higher risk, 35 to 49 were at a 1.7 times higher risk, and 50 years and older were at a 1.9 times higher risk of suicide than their female Canadian counterparts. However, these estimates were not statistically significantly different from each other, and suggest that overall, the risk of suicide remains elevated over a female Veteran’s lifetime, and may even increase with time when controlling for other factors, as discussed in the time since release section that follows.
Similar to these findings, the 2017 VSMS found that both female Veterans under 45 and 45 years and older had an approximately 1.8 times higher risk of suicide compared to other female Canadians (Simkus, VanTil, and Pedlar, 2017; VanTil, Simkus, Rolland-Harris, 2018), further reinforcing that age does not appear to be a risk factor for suicide in female Veterans.
Females by time since release
In contrast to males, the rate of suicide in female Veterans was initially significantly lower than as seen in Canadian females, but then 10 to 20 years after release, it increased significantly and was significantly higher than the female general population. Eventually, after 20 years, the female Veteran suicide rate decreased again to be similar to that of their female Canadian counterparts. These findings may also explain why age at death and age at release were not significantly associated with suicide in the female VSMS cohort, because unlike males, female Veterans are not as likely to die by suicide at a younger age in the immediate years after release.
This is the first time this trend has been observed using Canadian female Veteran data, and at this time is not fully understood. These findings will be further explored in conjunction with other research on female Veteran suicidality and mental health to better understand why female Veterans differ from their male counterparts.
Study strengths
Many of the strengths of the VSMS have been discussed previously in the 2017 Technical Report (Simkus, VanTil, and Pedlar, 2017). A summary, however, is provided below.
Firstly, DND administrative data were used to develop a large 200,000-person cohort over a period of nearly 40 years of study time. The size of cohort allowed for studying suicide, a relatively rare health event, and collect statistically significant findings, something that has been challenging in the past. In addition, the amount of data analysed for this study allows us to examine female Veterans, who are often excluded from or combined with male populations in military suicide analyses due to small numbers. The findings from both the 2018 and 2017 VSMS have provided evidence that the suicide behaviours and risk factors in female Veterans are different from male Veterans, providing the rationale to support prevention and treatment efforts targeted specifically to females.
Secondly, the data used in the VSMS is high quality. Using pay data allowed for a natural built-in feedback mechanism to correct errors, and mortality data came from official death records from the provinces and territories. In addition, this study is a complete census of all Veterans who released between 1976 and 2012, and not a sample, ensuring that it is highly representative of the CAF Regular Force and Reserve Class C Force Veteran population. There was also a high linkage rate between the military data and the mortality data (Rolland-Harris et al., In Press), resulting in a high level of confidence that nearly all deaths have been accounted for in this study.
Lastly, the cohort study design allowed for the investigation of not only newer Veterans, but also Veterans who released from the CAF as far back as 1976. As a result, suicide trends over the past four decades were able to be examined, and the number of years between release and suicide could be studied to identify when Veterans are at highest risk. As a comparison, after a review of the international literature, we were unable to find another study that examined time since release as a risk factor beyond 12 years.
Study limitations and opportunities for future research
Although suicidality is complex and multi-factorial in nature, the VSMS is limited to analysing only data available at time of release. Data on other possible variables associated with risk of suicide, such as ethnicity, sexual orientation, marital status, employment, income, education, and underlying physical and mental health conditions (PHAC, 2016; Thompson et al., 2016), were not available for this study. The LASS has consistently found a higher prevalence of mental and physical health problems among released CAF Regular Force and Reserve Class C Veterans (VanTil et al., 2017; Thompson et al., 2016; VanTil et al., 2016), which is consistent with VSMS findings. Unfortunately problems during life that could result in a suicide are difficult to examine in the same study design as deaths.
Expanding on the previous limitation, the VSMS data captured only deaths by suicide, not medical data. As a result, this study does not examine medical risk factors associated with suicide, nor does it examine suicidal ideation nor suicide attempts. To put this into context, an estimated 3.2% of suicide attempts in American adults are fatal (Han et al., 2016), similar to estimates that approximately 5% of suicide attempts worldwide are fatal (WHO, 2014). In addition, 8% of Canadian Regular Force Veterans had past-year suicidal ideation (VanTil et al., 2017). As a result, the deaths captured in this study represent only a small proportion of those Veterans who experience suicidality.
Complete military history is not available for all Veterans in this study cohort, and therefore the study is limited to military information available at the time of release from the CAF. VAC continues to work with DND to examine service-related risk factors as part of the joint ongoing CF CAMS 2, such as deployment history, length of service, and occupations within the CAF.
Class A and B Reservists were not included in the military cohort. However, these excluded Veterans have similar characteristics as the general population, including similar rates of depression, anxiety, activity limitations, social support, and satisfaction with life. This suggests that they were appropriately included in the general population instead of being combined with the Reserve Class C population (VanTil et al., 2016).
Personnel who had both Regular Force and Reserve Force Class C service time were combined to improve the statistical power of the study. However, small numbers of Reserve Class C service may have had Regular Force service that pre-dated 1976.
Reason for release utilized administrative release codes that demonstrated inconsistent use over the past four decades. There was a large shift in the proportion of CAF personnel who had involuntary releases prior to the 1990s to a larger proportion of medical releases in the 1990s and 2000s. This may be related to changes to medical policy where it became easier for serving personnel who recover from a mental disorder to remain in service, and thereby increasing care seeking and reducing career-related barriers (Boulos and Zamorski, 2016b). There is also ambiguity of the voluntary nature of releases coded as either involuntary or voluntary, so that the codes may not reflect the reason for release. This study was unable to examine reason for release as a risk factor in females as the number of suicides in the partial 1992 to 2012 female cohort was too small and failed to meet STC privacy guidelines.
Finally, there is an approximate four-year delay at STC to obtain complete mortality data from the provinces and territories for linkage to other datasets. Although the 2017 VSMS found that suicide rates did not increase significantly from 1976 to 2012, additional years of data will be added to the cohort as they become available.
Implications for prevention
The VAC-DND Joint Suicide Prevention Strategy (JSPS) describes the suicidal pathway, with opportunities for intervention. The strategy also aims to prevent suicide in CAF personnel and Veterans by continuously improving data collection, recognizing system gaps, and improving service delivery (CAF-VAC, 2017). Based on the findings of the 2018 VSMS, several considerations are recommended for the strategy when developing policies and delivering services to CAF Veterans.
Firstly, interventions and suicide prevention should be more accessible for NCMs, males who release before the age of 45, and Veterans with a non-voluntary release.
Secondly, suicide prevention should not be focused on only the immediate period after release from the CAF, and mental health support and other interventions should be available for decades after release. VAC has conducted significant research on military to civilian transition and has found that recent-era Veterans differed from Canadians more than earlier-era Veterans when examining several health indicators, including self-rated mental health (VanTil, McLean, and Sweet, 2018). These patterns suggest that, with time, Veterans adopt many of the health characteristics and behaviours of their civilian counterparts as they re-integrate into the civilian community. The VSMS observed that this may take more than 20 years. In addition, to the best of our knowledge, these findings highlight for the first time that female Veterans exhibit very different suicide patterns from males, and suicide prevention strategies should take into account their differing risk profiles.
Finally, the findings from the VSMS should be considered in conjunction with other research examining suicidality. This includes suicide rates while serving (Rolland-Harris, 2017), suicide ideation and attempts in Canadian Veterans (Thompson et al., 2014; Thompson et al., 2016), and international research in this area. The broader discussion on integration of suicidality findings in both serving military populations and released Veterans with prevention strategies is now underway (Thompson et al., Submitted).
Conclusions
The 2018 VSMS was able to identify several risk factors for suicide in CAF Veterans, in addition to changes in suicide risk over time after release from the CAF.
For male CAF Veterans, younger age at release, Junior NCM rank, and non-voluntary release were most strongly associated with increased risk of suicide. Reserve Class C and Regular Force Veterans had a similar risk of suicide. The risk of suicide was greatest approximately four years after release from CAF. This risk decreased with time until approximately 20 years after release when the male Veteran suicide rate was similar to that of the rest of the male Canadian population.
Female Veterans who released as NCMs were at greatest risk of suicide. Suicide risk did not vary significantly with age at release nor age at death. Similar to males, there was no significant difference in suicide risk between female Class C Reservist and Regular Force Veterans. In contrast, however, female Veterans’ risk of suicide continued to increase for many years after they had released from the CAF. Initially at release, they had a lower rate of suicide than the female general population, but this rate increased to be higher than the female general population in the second decade after release, and, like male Veterans, it was not until approximately 20 years after release that the suicide rate decreased again to similar levels as female Canadians.
VAC is committed to the well-being of Canadian Veterans, and preventing suicides is a top public health priority for the department. VAC will continue to support research to better understand suicide, and provide evidence to inform suicide prevention activities and interventions.
List of Acronyms
- AIHW
- Australian Institute of Health and Welfare
- CAF
- Canadian Armed Forces
- CCPS
- Central Computerised Pay System
- CF CAMS
- Canadian Forces Cancer and Mortality Study
- CF CAMS 2
- Canadian Forces Cancer and Mortality Study 2
- CGP
- Canadian General Population
- CI
- Confidence Interval
- CVSD
- Canadian Vital Statistics Database
- DND
- Department of National Defence (Canada)
- HR
- Hazard Ratio
- HRMS
- Human Resources Management System
- ICD
- International Classification of Disease
- JSPS
- VAC-DND Joint Suicide Prevention Strategy
- LASS
- Life After Service Study
- NCM
- Non-commissioned member
- PHAC
- Public Health Agency of Canada
- PTSD
- Posttraumatic Stress Disorder
- PY
- Person-years
- SMR
- Standardised Mortality Ratio
- STC
- Statistics Canada
- UK
- United Kingdom
- US
- United States
- VAC
- Veterans Affairs Canada
- VSMS
- Veteran Suicide and Mortality Study
- WHO
- World Health Organisation
References
Australian Institute of Health and Welfare. (2017). Incidence of suicide among serving and ex-serving Australian Defence Force personnel: Detailed analysis 2001-2015. Cat. no. PHE 218. Canberra: AIHW.
Boulos, D., Zamorski, M.A. (2016a). Contribution of the mission in Afghanistan to the burden of past-year mental disorders in Canadian Armed Forces personnel, 2013. Can J Psychiat. 61(Supplement I):64S-76S.
Boulos, D., Zamorski, M.A. (2016b). Delay to mental healthcare in a cohort of Canadian Armed Forces personnel with deployment-related mental disorders, 2001-2011; a retrospective cohort study. BMJ Open. 6:e012384.
Canadian Armed Forces and Veterans Affairs Canada. (2017). Canadian Armed Forces and Veterans Affairs Canada Joint Suicide Prevention Strategy. Retrieved from https://www.canada.ca/content/dam/dnd-mdn/documents/reports/2017/caf-vac-joint-suicide-prevention-strategy.pdf
Han, B., Kott, P.S., Hughes, A., McKeon, R., Blanco, C., Compton, W.M. (2016). Estimating the rates of deaths by suicide among adults who attempt suicide in the United States. J Psychiat Res. 77: 125-133.
Kapur, N., While, D., Blatchley, N., Bray, I., Harrison, K. (2009). Suicide after leaving the UK Armed Forces – a cohort study. PLoS Medicine. 6(3):e1000026
Lee, J.E.C., Hachey, K.K. (2011). Descriptive Analyses of the Recruit Health Questionnaire: 2007-2009. National Defence. Defence R&D Canada and Director General Military Personnel Research and Analysis. Ottawa, Canada.
MacLean, M.B., Clow, B., Ralling, A., Sweet, J., Poirier, A., Buss, J., Pound, T., Rodd, B. (2018). Veterans in Canada released since 1998: A Sex-disaggregated Profile, Veterans Affairs Canada, Research Technical Report, 24 September 2018.
Navaneelan, T. (2016). Suicide rates: an overview. Health at a Glance, Statistics Canada. Retrieved from https://www.statcan.gc.ca/pub/82-624-x/2012001/article/11696-eng.htm
Pearson, C., Zamorski, M.A., Janz, T. (2014). Mental health of the Canadian Armed Forces. Catalogue no. 82-624-X. Statistics Canada. Ottawa, Canada.
Public Health Agency of Canada. (2016). Working together to prevent suicide in Canada: The federal framework for suicide prevention. Retrieved from: https://www.canada.ca/content/dam/canada/public-health/migration/publications/healthy-living-vie-saine/framework-suicide-cadre-suicide/alt/framework-suicide-cadre-suicide-eng.pdf
Reger, M.A., Smolenski, D.J. Skopp, N.A., Metzger-Abamukang, M.J., Kang, H.K., Bullman, T.A., Perdue, S., Gahm, G.A. (2015). Risk of suicide among US military service members following Operation Enduring Freedom or Operation Iraqi Freedom deployment and separation from the US military. JAMA Psychiat. 72(6):561-569.
Rolland-Harris, E., VanTil, L., Zamorski, M., Boulos, D., Reicker, A., Trudeau, R., Masoud, H., Weeks, M., Simkus, K. (2018a). The Canadian Forces Cancer and Mortality Study II: A Longitudinal Record-Linkage Study Protocol. Can Med Assoc J., DOI: 10.9778/cmajo.20170125
Rolland-Harris, H., Weeks, M., Simkus, K., VanTil, L. (2018b). Overall mortality of Canadian Armed Forces personnel enrolled 1976-2012. Occ Med. 68(1):32-37. DOI:10.1039/occmed/kqx182
Rolland-Harris, H. (2017). 2017 Report on Suicide Mortality in the Canadian Armed Forces (1995 to 2016). Surgeon General Report. Department of National Defence. Ottawa, Canada.
Shen, Y., Cunha, J.M., Williams, T.V. (2016). Time-varying associations of suicide with deployments, mental health conditions, and stressful life events among current and former US military personnel: a retrospective multivariate analysis. Lancet Psychiat. 3(11):1039-1048.
Simkus, K., VanTil, L., Pedlar, D. (2017). 2017 Veteran Suicide Mortality Study: 1976 to 2012. Charlottetown (PE): Veterans Affairs Canada, Research Directorate Technical Report; November 30, 2017. Avail: http://publications.gc.ca/pub?id=9.847961&sl=0
Statistics Canada. (2011). Canadian Forces Cancer and Mortality Study: Causes of Death. In: Statistics Canada, ed. Ottawa: Minister of Industry.
Thompson, J.M., Heber, A., Carrese, L., VanTil, L., Simkus, K., Sareen, J., Pedlar, D. (Submitted). Life course well-being framework for suicide prevention in Canadian Armed Forces Veterans. JMVFH, Submitted.
Thompson, J.M., VanTil, L., Zamorski, M.A., Garber, B., Dursun, S., Fikretoglu, D., Ross, D., Richardson, J.D., Sareen, J., Sudom, K., Courchesne, C., Pedlar, D. (2016). Mental health of Canadian Armed Forces Veterans – Review of Population Studies. JMVHR. 2(1):70-86.
Thompson J.M., Zamorski, M.A., Sweet, J., VanTil, L.D., Sareen, J., Pietrzak, R.H., Hopman, W.H., MacLean, M.B., Pedlar, D.J. (2014). Roles of physical and mental health in suicidal ideation in Canadian Armed Forces Regular Force veterans. C J Public Health. 105(2):e109-e115.
VanTil, L.D., Simkus, K., Rolland-Harris, E. Pedlar, D. (2018). Veteran suicide mortality in Canada from 1976 to 2012. JMVFH. 4(2):110-116. DOI: 10.3138/jmvfh.2017-0045
VanTil, L.D., McLean, M.B., Sweet, J., McKinnon, K. (2018). Understanding future needs of Canadian veterans. Health Rep. 29(11):20-25.
VanTil, L., Sweet, J., Poirier, A., McKinnon, K., Sudom, K., Dursun, S., Pedlar, D. (2017). Well-Being of Canadian Regular Force Veterans, Findings from LASS 2016 Survey. Charlottetown PE: Veterans Affairs Canada. Research Directorate Technical Report, 23 June 2017. Avail: http://publications.gc.ca/pub?id=9.839366&sl=0
VanTil, L., MacLean, M.B., Poirier, A., McKinnon, K., Keough, J., Sudom, K., Dursun, S., Herron, M., Pedlar, D. (2016). Veterans of the Reserve Force: Life After Service Studies 2013. Veterans Affairs Canada, Research Directorate Technical Report (21). Retrieved from http://publications.gc.ca/pub?id=9.826344&sl=0
World Health Organisation. (2014). Preventing suicide: A global imperative. WHO. Geneva, Switzerland.
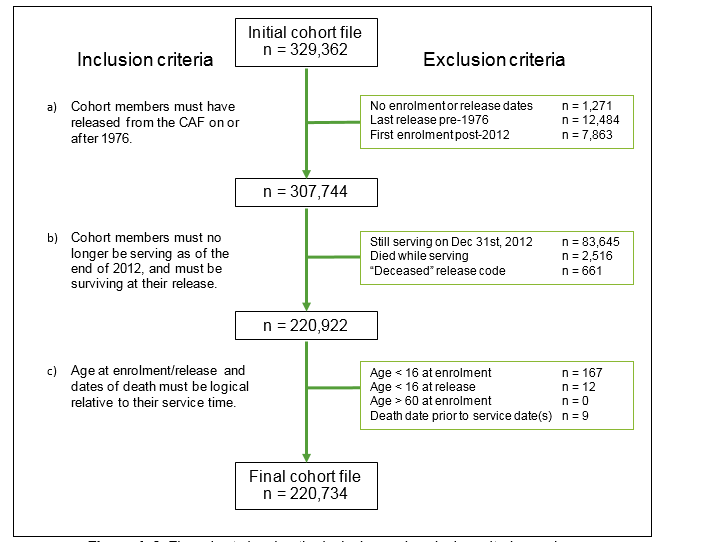
Appendix A – Cohort Definition
The VSMS follows CAF Regular Force and Class C Reservist Veterans who released from the CAF between January 1, 1976 and December 31, 2012. The cohort was defined using pay data from DND’s Central Computerised Pay System (CCPS) and death records from Statistics Canada’s Canadian Vital Statistics Database (CVSD) under the following inclusion criteria:
- cohort members must have released from the CAF on or after 1976;
- cohort members must no longer be serving as of December 31, 2012, and must be surviving upon their release (i.e. did not die in service); and
- their age at enrolment/release and dates of death must be logical relative to their service time.
The cohort grew from 9,885 Veterans in 1976 to a total 220,734 Veterans by 2012 (Figure A-1). This does not exclude Veterans who died during this period, although Veterans were removed from the study population as they died to calculate SMRs and rates.
Figure A-1. Cumulative frequency of new Veterans entering the VSMS cohort, 1976 to 2012.
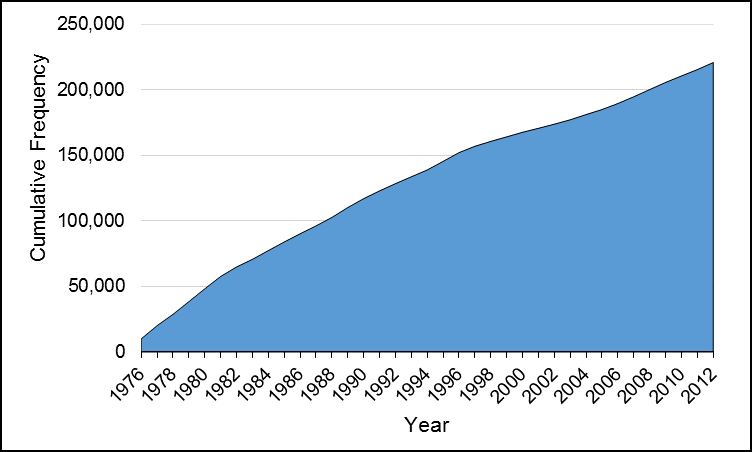
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Given that Reserve A and B personnel are paid through a different system, this precludes the inclusion of Class A and B reservists from this study.
Where possible, data were cleaned, and where corrections could not be made, exclusion criteria were applied. This included setting 16 years as a minimum age at enrolment and release, and 60 years as a maximum age of enrolment. Any personnel who had a death record and died within 14 days after release were considered “in-service deaths” instead of Veteran deaths due to the more likely possibility of the release date being entered incorrectly; this was supported based on the number of suicides within 14 days of release aligning with the known number of in-service suicide deaths from previous DND studies. In addition, any CAF personnel who had “deceased” as their reason for release were excluded from the cohort, whether or not they had a death record in the linked cohort. In all cases, these data quality exclusions were relatively rare and it would be unlikely that their exclusion from the cohort would affect the results (Figure A-2). The final cohort file contained the military career history of 220,734 unique individuals.
Figure A-2. Flow chart showing the inclusion and exclusion criteria used to create the VSMS cohort.
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Appendix B – Data Sources
The Central Computerised Pay System (CCPS) is an electronic DND dataset which identifies all Regular Force and Class C Reservists (those reservists who participated in international operations and/or tours of duty) who enrolled and/or released from the CAF dating back to 1976. CCPS was chosen to create the cohort as it has an accuracy and precision advantage from its built-in feedback mechanism, whereby both personnel and the employer are motivated to correct pay errors as soon as possible. Salaries and pay amounts were not shared with the research team; only start and end dates of pay were used to identify when each service member ended their employment with the CAF (“released”), in addition to the start and end dates for any extra deployment-associated pay they would have received when overseas.
The Human Resources Management System (HRMS) is a second DND administrative dataset that contains historical and current demographic and occupational data on serving CAF personnel. The cohort file defined using CCPS was supplemented and validated using data from HRMS. This aided to reduce the amount of missing information and resolving incorrect information.
The Canadian Vital Statistics Database (CVSD) provides mortality information from 1950 onwards to the latest available year of data, which at the time of data linkage for the VSMS, was 2012. Information from the CVSD is provided by the ICD code in effect at the time of death. Cause of death information is recorded by Vital Statistics Registries in the provinces and territories. The mortality variables used in the VSMS are full date of death, and underlying cause of death (ICD code).
The CAF personnel data from DND were deterministically linked by STC to the CVSD based primarily on Social Insurance Number. The anonymised linked data were held in a secure area within STC and were accessible only to designated researchers at DND and VAC. Further details on the data and linkage methodology are published under the CF CAMS 2 protocol, which uses the same linked data as the VSMS (Rolland-Harris et al., In Press).
Aggregate Canadian population data and death data were provided by STC in the form of historical reports, spreadsheets, and CANSIM tables available publicly online. Population counts and death counts were provided by sex, five-year age groups, year, and ICD-8, -9, or -10 codes for cause of death.
Appendix C – Definition of Cases and Military Variables
Suicide deaths were reported using three different versions of the WHO’s International Classification of Diseases (ICD) throughout the 37-year study: for ICD versions 8 (years 1976 to 1978) and 9 (years 1979 to 1999), codes E950-E959 were used; for ICD version 10 (years 2000 to 2012), codes X60-X84 and Y87.0 were used. This case definition is consistent with that used by both DND and STC when studying suicide (Rolland-Harris, 2016; Navaneelan, 2016).
Other specific or chapter-level causes of death in Veterans were not examined under the scope of the VSMS, although these topics are covered under DND’s Canadian Forces Cancer and Mortality Study 2 (CF CAMS 2) (Rolland-Harris et al., In Press; Rolland-Harris et al., 2018).
Release date was the final date the Veteran was paid by CCPS. This date was used to calculate age at release, and to calculate years since release.
Rank at release was recorded in DND administrative data using 19 ranksFootnote 1, plus Recruits. The ranks have different titles for the Army/Air than for the Navy. This study categorized them into four groups:
- Senior Officer (Generals, Colonels, Majors and their Navy equivalents);
- Junior Officer (Captains, Lieutenants, Officer Cadets and their Navy equivalents);
- Senior Non-Commissioned Member (Warrant Officers, Sergeants and their Navy equivalents);
- Junior Non-Commissioned Member (Corporals, Privates, Recruits and their Navy equivalents).
Reason for release was recorded in DND administrative data using 17 release type codesFootnote 2. This study categorized the codes into 3 groups:
- Voluntary: 4a, 4b, 4c, 5a, 5c;
- Medical: 3a, 3b;
- Involuntary: 1a, 1b, 1c, 1d, 2a, 2b, 5b, 5d, 5e, 5f.
The term “non-voluntary release” was also used to describe any of the medical or involuntary codes.
Appendix D – Data Analysis
Privacy Regulations
In compliance with the requirements of the Statistics Act, all counts of deaths fewer than 10 are required to be suppressed. Therefore, where required, age groups or time periods were collapsed to ensure death counts were greater than or equal to 10. Where it was not possible to collapse subgroups, counts or rates were suppressed.
Standardised Mortality Ratios
Standardised mortality ratios (SMR) were used to compare the rate of suicide of the VSMS cohort with that of the CGP. Suicide rates were calculated separately for males and females, each time period of follow-up, and each age group in the VSMS cohort and compared with the corresponding group in the general population using indirect standardisation methods.
An SMR value of 1.0 indicates that the observed mortality in the Veteran cohort was the same as that observed in the CGP. Values less than 1.0 suggest lower mortality in the Veteran cohort while values greater than 1.0 suggest higher than expected mortality in the Veteran cohort. In addition to the point estimate, 95% confidence intervals (CI) were calculated, which are valuable in illustrating the expected random variability that is possible when dealing with small numbers of cases. Calculation of CIs used either normal approximation (death counts ≥ 100) or the exact Poisson method (death counts < 100). SMR CIs that overlap 1.0 were considered to be not statistically significant. See Figure D for a visual example of interpreting SMRs and their CIs.
Figure D. Example on how to interpret standardised mortality ratios (SMRs) and their corresponding confidence intervals (CIs).
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Age-adjusted rates
Age-adjusted suicide rates for both Veterans and the CGP were calculated using direct standardisation with the 2012 CGP of Canadians aged 15 and older as a reference for examining suicide rate by time since release from the CAF. It should be noted that small numbers of deaths (the numerator) and/or small population (the denominator) can lead to statistically unstable rates, particularly for those Veterans who have been released from the CAF for several decades. For rates, 95% CIs were calculated using either normal approximation (death counts ≥ 100) or the exact Poisson method (deaths counts < 100).
Cox proportional hazards model:
Cox models generate hazards ratios, which represent the relative death rate and can be interpreted in terms of relative risk compared to a reference category. As an example, if females were the reference category, an HR of 2.0 for males would imply that the relative risk of death was twice as high among males as it was among females. Conversely, an HR of 0.5 for males would imply that males had a risk of death half that of females. An HR of 1.0 would indicate that both males and females had a similar risk. 95% confidence intervals (CI) were also calculated; CIs that overlap 1.0 suggest that the HR is not statistically significant. For each model, multivariate-adjusted HRs were calculated control for the other variables.
The variables that were included in the models were component at release, rank at release, age at release, and reason for release. As the intent of the model was to conduct a descriptive analysis rather than generate a predictive model, all variables were included in the models, whether or not they were statistically significant. No significant interaction terms were identified. The decision on how to create categories for these variables was based on a combination of respecting minimum cell counts required by STC, in addition to selecting the categorisations with the lowest p-values upon univariate analysis while maintaining as much granularity as possible. Year of release was not included in the models for two reasons: 1) because the 2017 VSMS determined that the risk of suicide had not changed significantly over the 37 years of the study, and 2) because year of release is highly collinear with time since release. Variables such as length of service, occupation, and deployment history are not available for the VSMS analyses as complete military histories are not available for all Veterans in the cohort; therefore analysis of variables related to military service time will be conducted as part of the joint VAC/DND Canadian Forces Cancer and Mortality Study 2, which includes only serving and released CAF personnel for whom complete military histories are available.
Violations of the proportionality assumption were tested for using Schoenfeld and scaled Schoenfeld residuals and global proportional-hazards tests. (Appendix H). The only violation of the proportionality assumption occurred when both males and females were included in the same model. As a result, models were developed separately for each sex.
Goodness-of-fit of each model was assessed using Cox-Snell residuals and comparing to the Nelson-Aalen cumulative hazard function (Appendix H). The model fits the data well when the Nelson-Aalen cumulative hazard function follows the 45 degree line generated by the Cox-Snell residuals, and all models presented here fit the data well. In this report, Nelson-Aalen cumulative hazard functions were smoothed to protect privacy by the elimination of obvious steps to avoid the possibility of deriving the number of suicides at any given time in the study.
Survival functions
The Cox proportional hazard model generates survival functions to visually portray the probability of “surviving” (i.e. not experiencing an event) to time t. A flat survival curve that remains close to 1.0 implies very good survival, while a survival curve that drops sharply toward 0 implies poor survival. Note that the proportion of the cohort “surviving” does not always equal the proportion who are alive, but the proportion who are alive and therefore at risk of experiencing the event. It should be noted that the right ends of the curves may show some variability due to reduced effective sample caused by prior failures and censoring. Survival curves have been smoothed to eliminate obvious steps, and therefore the possibility of deriving the number of suicides at any given time in the study, and therefore protect privacy.
Hazard functions
The Cox proportional hazard model also generates smoothed hazard functions, or hazard rates, which visually represent the instantaneous risk of an event at time t. Hazard functions provide useful information on how risk of an event changes over time, and the relative risk of the event when comparing between groups. If the hazard function remains constant over time, this would mean that the risk of the event did not change over the time period. A peak in the curve is known as a prolongation point; before this time point, the rate of the event continues to increase, and after the point, the rate of the event begins to decline. If at a time interval the hazard function equalled 2.0, this would mean that one would expect 2.0 events to occur in a time interval that is one unit long. If at a time period males had a hazard rate of 2.0 and females had a hazard rate of 1.0, then at that point in time, males had twice the rate of the event as females. However, as none of the models presented here violated the proportionality assumption, these hazard rate ratios remain generally constant over time and can be generalized by the global HRs generated by the Cox model regressions discussed previously.
Smoothed hazard curves are truncated at either end of the study time because the smoothing requires averaging values over the moving window of data; therefore, the end points contain insufficient data for accurate estimation. It should be noted that the right ends of the curves may show some variability due to reduced effective sample caused by prior failures and censoring.
Software
All data cleaning, manipulation, and analysis activities were conducted using Stata 14 and Microsoft Excel. Data linkage activities were conducted using SAS 9.3.
Appendix E – Age and sex distribution of the Veteran study cohort
| Male | Female | |||
|---|---|---|---|---|
| n | % | n | % | |
| Total in cohort | 197,249 | 23,489 | ||
| Age at 31 Dec 2012 (still alive) | ||||
| < 25 years | 3,284 | 1.9% | 439 | 1.9% |
| 25 – 34 | 11,980 | 6.8% | 1,778 | 7.8% |
| 35 – 44 | 22,781 | 12.8% | 3,794 | 16.6% |
| 45 – 54 | 68,798 | 38.8% | 10,845 | 47.5% |
| 55 – 64 | 37,045 | 20.9% | 5,249 | 23.0% |
| 65+ | 33,443 | 18.9% | 738 | 3.2% |
| Total | 177,331 | 100.0% | 22,843 | 100.0% |
| Mean age | 70.8 years | 59.1 years | ||
| Age at death (all cause) | ||||
| < 25 years | 435 | 2.2% | 15 | 2.3% |
| 25 – 34 | 1,115 | 5.6% | 68 | 10.6% |
| 35 – 44 | 1,623 | 8.1% | 136 | 21.2% |
| 45 – 54 | 3,253 | 16.3% | 229 | 35.7% |
| 55 – 64 | 4,662 | 23.4% | 112 | 17.4% |
| 65+ | 8,830 | 44.3% | 82 | 12.8% |
| Total | 19,918 | 100.0% | 642 | 100.0% |
| Mean age | 60.0 years | 49.6 years | ||
Appendix F – Supplemental Cox proportional hazard model tables
| Variable | Multivariable-adjusted hazard ratios (95% CI) | |
|---|---|---|
| Sex | Male | 2.82 (2.19-3.61)* |
| Female | Reference | |
| Component | Any RegF service | 1.05 (0.85-1.29) |
| Only ResC service | Reference | |
| Rank at release | Junior NCM | 1.93 (1.59-2.35)* |
| Senior NCM | 1.34 (1.00-1.79) | |
| Junior Officer | Reference | |
| Senior Officer | 0.91 (0.55-1.52) | |
| Age at release | < 25 | 2.83 (2.18-3.67)* |
| 25-34 | 2.12 (1.61-2.79)* | |
| 35-44 | 1.47 (1.14-1.90)* | |
| 45+ | Reference | |
* HR is significantly different than 1.
1 Violations of proportionality assumption on global model (p=0.0021), and on the sex variable (p=0.0005). Model fit data well (Appendix H).
| Variable | Multivariable-adjusted hazard ratios (95% CI) | |
|---|---|---|
| Sex | Male | 3.86 (2.05-7.27)* |
| Female | Reference | |
| Component | Any RegF service | Reference |
| Only ResC service | 0.97 (0.51-1.83) | |
| Rank at release | Junior NCM | 1.50 (1.01-2.22)* |
| Senior NCM | 1.26 (0.76-2.10) | |
| Junior Officer | Reference | |
| Senior Officer | 0.63 (0.25-1.58) | |
| Age at release | < 25 | 2.27 (1.35-3.82)* |
| 25-34 | 2.30 (1.41-3.77)* | |
| 35-44 | 1.93 (1.25-2.99)* | |
| 45+ | Reference | |
| Reason for release | Voluntary | Reference |
| Involuntary | 2.01 (1.45-2.79)* | |
| Medical | 1.69 (1.23-2.32)* | |
* HR is significantly different than 1.
1 Violations of proportionality assumption on global model (p=0.0428), and on the sex variable (p=0.0018). Model fit data well (Appendix H).
Appendix G – Additional survival functions from Cox proportional hazard models
Figure G1. Male Veteran smoothed survival function for risk of dying by suicide by component (Regular Force vs. Reserve Force Class C service only), 1976 to 2012 releases.
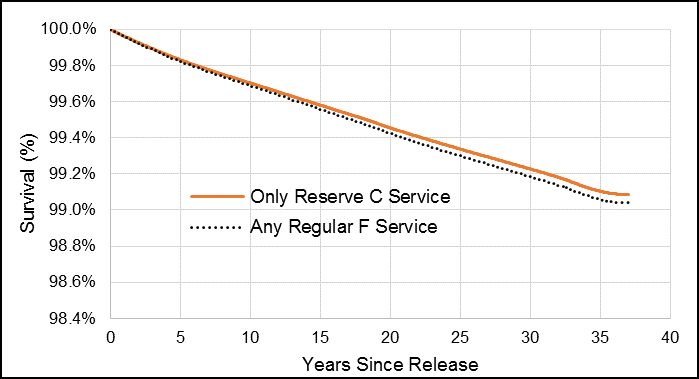
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G2. Male Veteran smoothed survival function for risk of dying by suicide by rank at release, 1976 to 2012 releases.
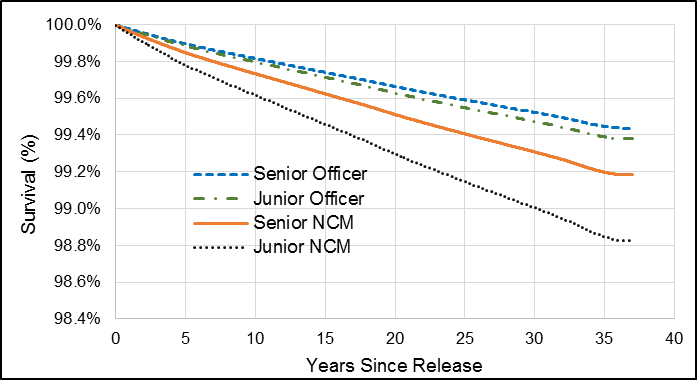
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G3. Male Veteran smoothed survival function for risk of dying by suicide by age at release, 1976 to 2012 releases.
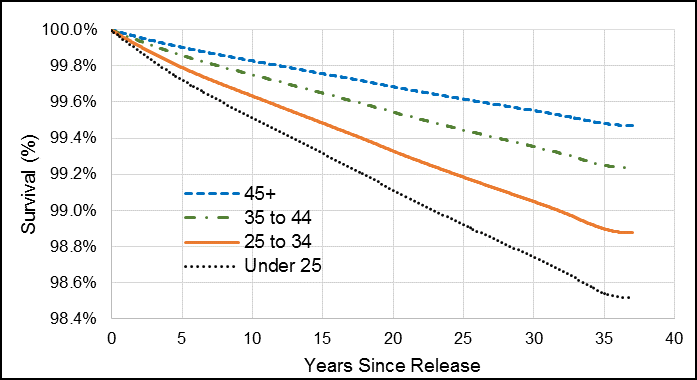
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G4. Male Veteran smoothed survival function for risk of dying by suicide by component (Regular Force vs. Reserve Force Class C service only), 1992 to 2012 releases.
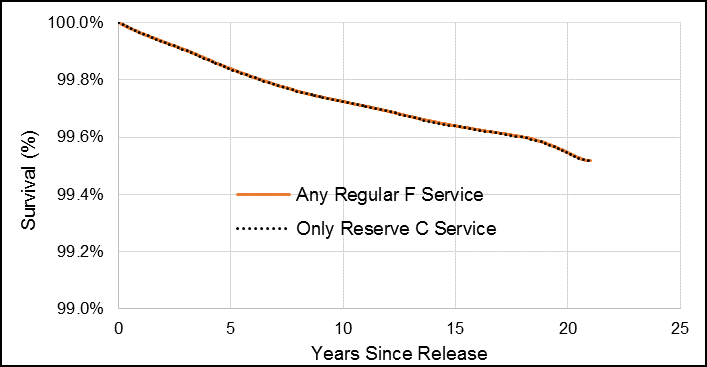
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G5. Male Veteran smoothed survival function for risk of dying by suicide by rank at release, 1992 to 2012 releases.
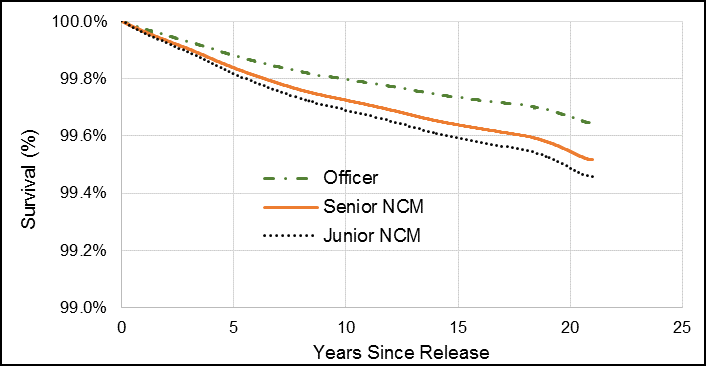
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G6. Male Veteran smoothed survival function for risk of dying by suicide by age at release, 1992 to 2012 releases.
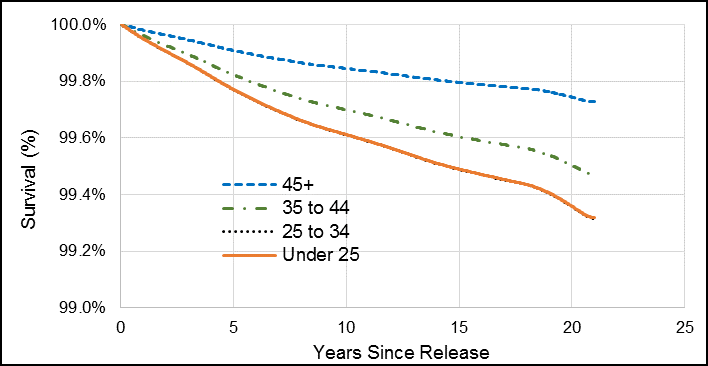
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G7. Male Veteran smoothed survival function for risk of dying by suicide by reason for release, 1992 to 2012 releases.
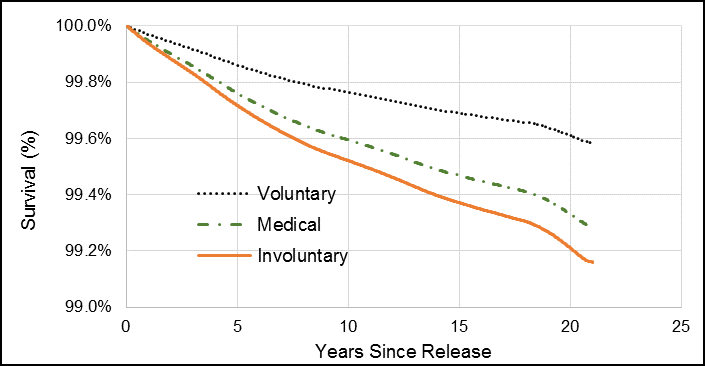
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G8. Female Veteran smoothed survival function for risk of dying by suicide by component (Regular Force vs. Reserve Force Class C service only), 1976 to 2012 releases.
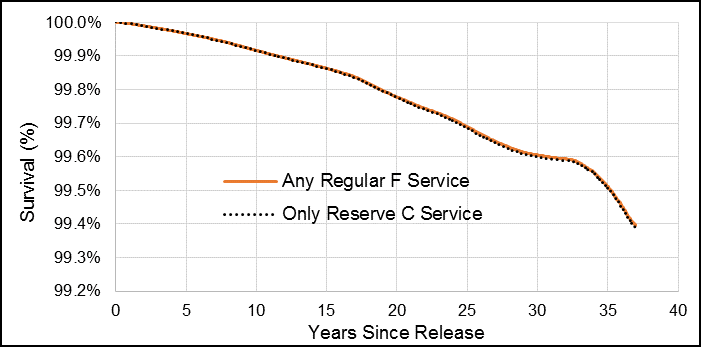
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G9. Female Veteran smoothed survival function for risk of dying by suicide by rank at release, 1976 to 2012 releases.
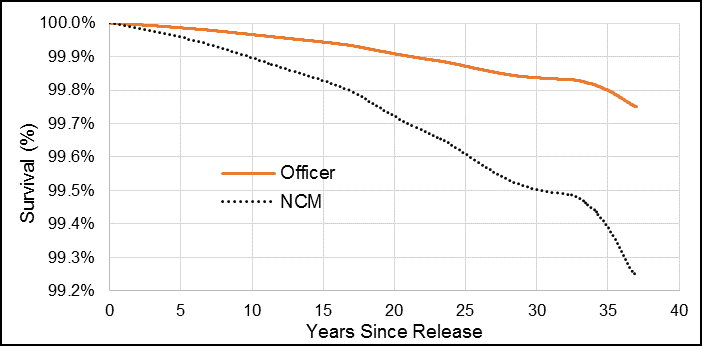
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Figure G10. Female Veteran smoothed survival function for risk of dying by suicide by age at release, 1976 to 2012 releases.
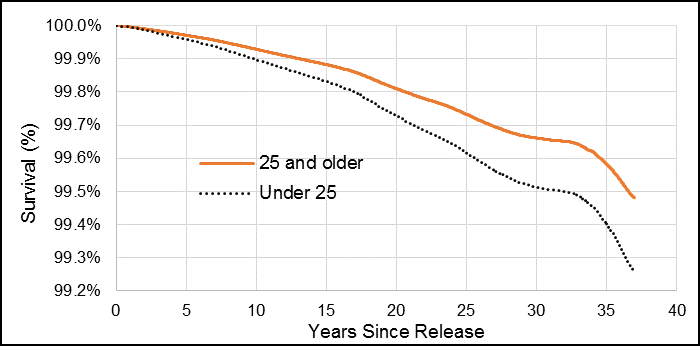
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Appendix H – Cox proportional hazards model fit
Veterans Cox proportional hazards model (1976-2012), both sexes combined
Schoenfeld and scaled Schoenfeld residuals tests showed that there was a violation of the proportionality assumption for the sex variable (p=0.0005). In addition, the overall model violated the proportional-hazards assumption (p=0.0021). Comparing the model’s Nelson-Aalen cumulative hazard function to the Cox-Snell residuals, it was observed that the model fit the data well, despite the proportional-hazards assumption violation (Figure H1).
Figure H1. Test for goodness-of-fit for 1976 to 2012 release male and female Veterans Cox proportional hazards model for suicide.
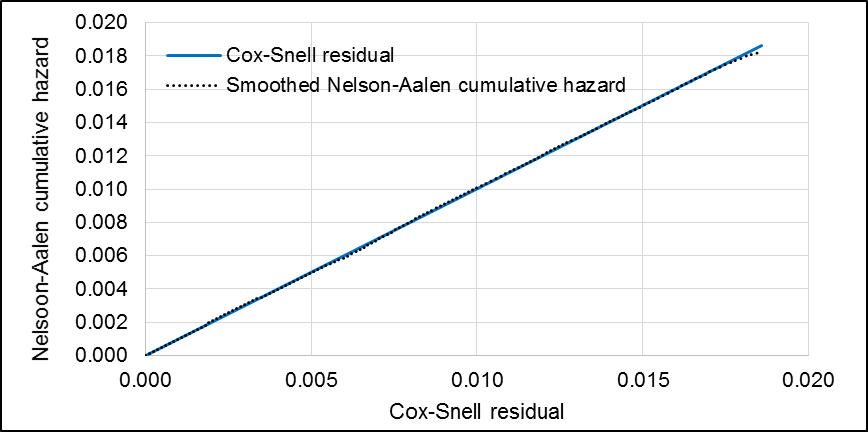
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Veterans Cox proportional hazards model (1992-2012), both sexes combined
Schoenfeld and scaled Schoenfeld residuals tests showed that there was a violation of the proportionality assumption for the sex variable (p=0.0018). In addition, the overall model violated the proportional-hazards assumption (p=0.0428). Comparing the model’s Nelson-Aalen cumulative hazard function to the Cox-Snell residuals, it was observed that the model fit the data well, despite the proportional-hazards assumption violation (Figure H2).
Figure H2. Test for goodness-of-fit for 1992 to 2012 release male and female Veterans Cox proportional hazards model for suicide.
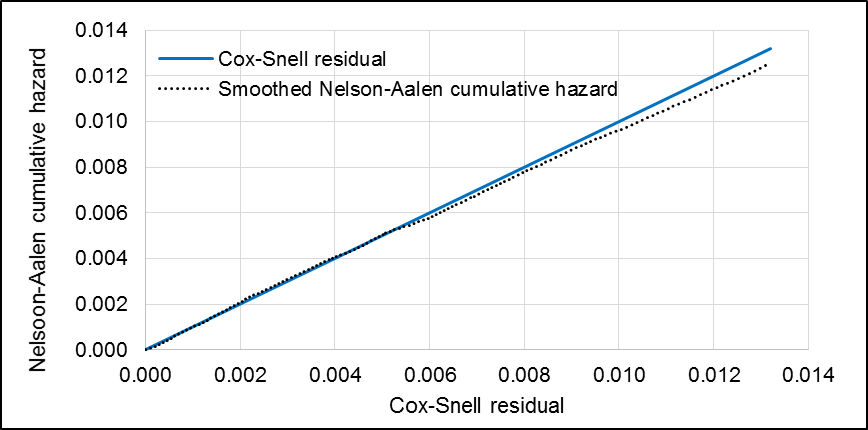
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Male Veterans Cox proportional hazards model (1976-2012)
Schoenfeld and scaled Schoenfeld residuals tests showed no violations of the proportionality assumption (p=0.2958). Comparing the model’s Nelson-Aalen cumulative hazard function to the Cox-Snell residuals, it was observed that the model fit the data well (Figure H3).
Figure H3. Test for goodness-of-fit for 1976 to 2012 release male Veterans Cox proportional hazards model for suicide.
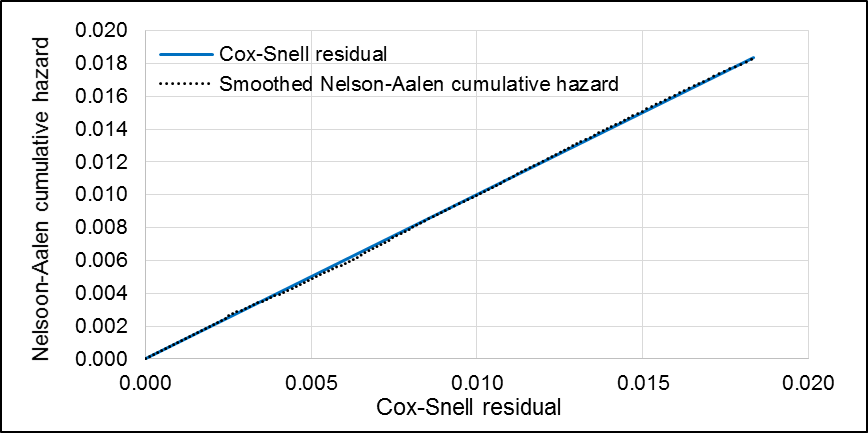
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Male Veterans Cox proportional hazards model (1992-2012)
Schoenfeld and scaled Schoenfeld residuals tests showed no violations of the proportionality assumption (p=0.8022). Comparing the model’s Nelson-Aalen cumulative hazard function to the Cox-Snell residuals, it was observed that the model fit the data well (Figure H4).
Figure H4. Test for goodness-of-fit for 1992 to 2012 release male Veterans Cox proportional hazards model for suicide.
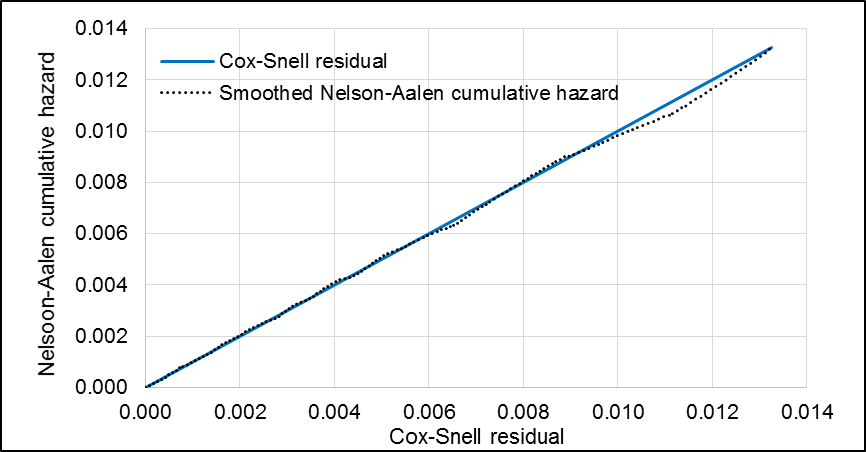
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Female Veterans Cox proportional hazards model (1976-2012)
Schoenfeld and scaled Schoenfeld residuals tests showed no violations of the proportionality assumption (p=0.8141). Comparing the model’s Nelson-Aalen cumulative hazard function to the Cox-Snell residuals, it was observed that the model fit the data fairly well (Figure H5).
Figure H5. Test for goodness-of-fit for 1976 to 2012 release female Veterans Cox proportional hazards model for suicide.
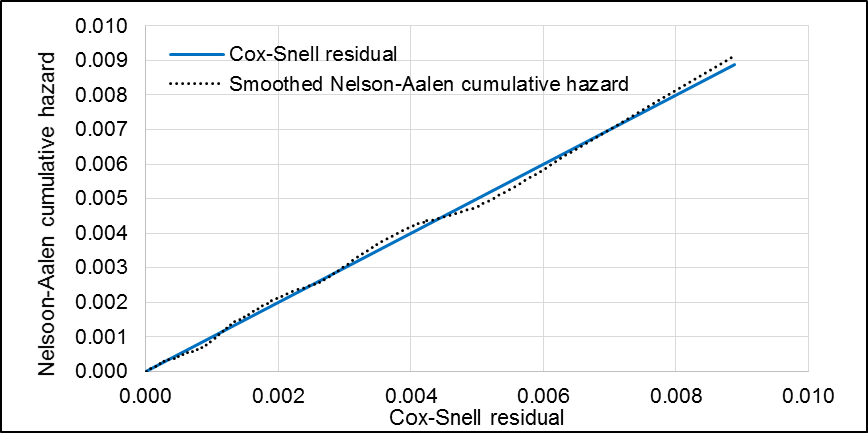
For more information, please contact VAC.Research-Recherche.ACC@canada.ca
Appendix I – Age-adjusted rates by time since release
| Years since release | Crude rate per 100,000 PY (95% CI) | Age-adjusted rate per 100,000 PY (95% CI) |
|---|---|---|
| 1 to 10 | 35.79 (32.99 - 38.58) | 27.48 (25.33 - 29.62) |
| 11 to 20 | 33.01 (29.95 - 36.07) | 23.76 (21.56 - 25.95) |
| 21+ | 33.66 (30.10 - 37.22) | 20.60 (18.42 - 22.78) |
| 2012 CGP | 20.62 | 20.62 |
| Years since release | Crude rate per 100,000 PY (95% CI) | Age-adjusted rate per 100,000 PY (95% CI) |
|---|---|---|
| 1 to 10 | 8.36 (4.87 - 13.38) | 3.85 (2.25 - 6.17) |
| 11 to 20 | 16.01 (10.26 - 23.83) | 12.99 (8.32 - 19.33) |
| 21+ | 22.15 (14.19 - 32.95) | 9.15 (5.86 - 13.62) |
| 2012 CGP | 6.4 | 6.4 |