Entitlement Eligibility Guideline (EEG)
Date reviewed: 25 July 2025
Date created: February 2005
ICD-11 code: 8C10.0
VAC medical code: 35400 Carpal tunnel syndrome
This publication is available upon request in alternate formats.
Full document – PDF Version
Definition
Carpal tunnel syndrome (CTS) is an entrapment neuropathy of the median nerve. The compression of the median nerve within the carpal tunnel of the wrist impairs sensation and can also affect the strength of the hand.
Note: CTS is distinct from other related disorders such as cumulative trauma disorders, repetitive strain injury of the wrist, or wrist tendinitis. These conditions, although occasionally sharing similar presentations, have different underlying causes from CTS and are considered separate medical conditions for entitlement purposes.
Diagnostic standard
Diagnosis by a qualified medical practitioner (orthopedic surgeon, plastic surgeon, neurologist, family physician), nurse practitioner, or physician assistant (within their scope of practice) is required.
Confirmation of CTS involves relevant investigations including electrophysiological testing, such as nerve conduction studies, and imaging assessments, such as ultrasound or magnetic resonance imaging (MRI) of the wrist.
Anatomy and physiology
The carpal tunnel is a narrow, anatomical passageway situated on the palm side of the wrist. It is formed by the wrist bones (carpal bones) on three sides and sealed by a strong band of connective tissue known as the transverse carpal ligament on the fourth side. This confined space accommodates the median nerve and the flexor tendons that bend the fingers (Figure 1: Carpal tunnel syndrome).
Originating from the brachial plexus in the neck, the median nerve traverses the arm and forearm to enter the hand through the carpal tunnel. It is crucial for providing sensation to the thumb, index, middle, and part of the ring fingers, in addition to supplying motor functions to the thumb's thenar muscles.
Inflammation or injury can lead to a reduction in the tunnel's space or an increase in its contents. This results in compression of the median nerve causing the sensory and motor disturbances characteristic of carpal tunnel syndrome.
Figure 1: Carpal tunnel syndrome
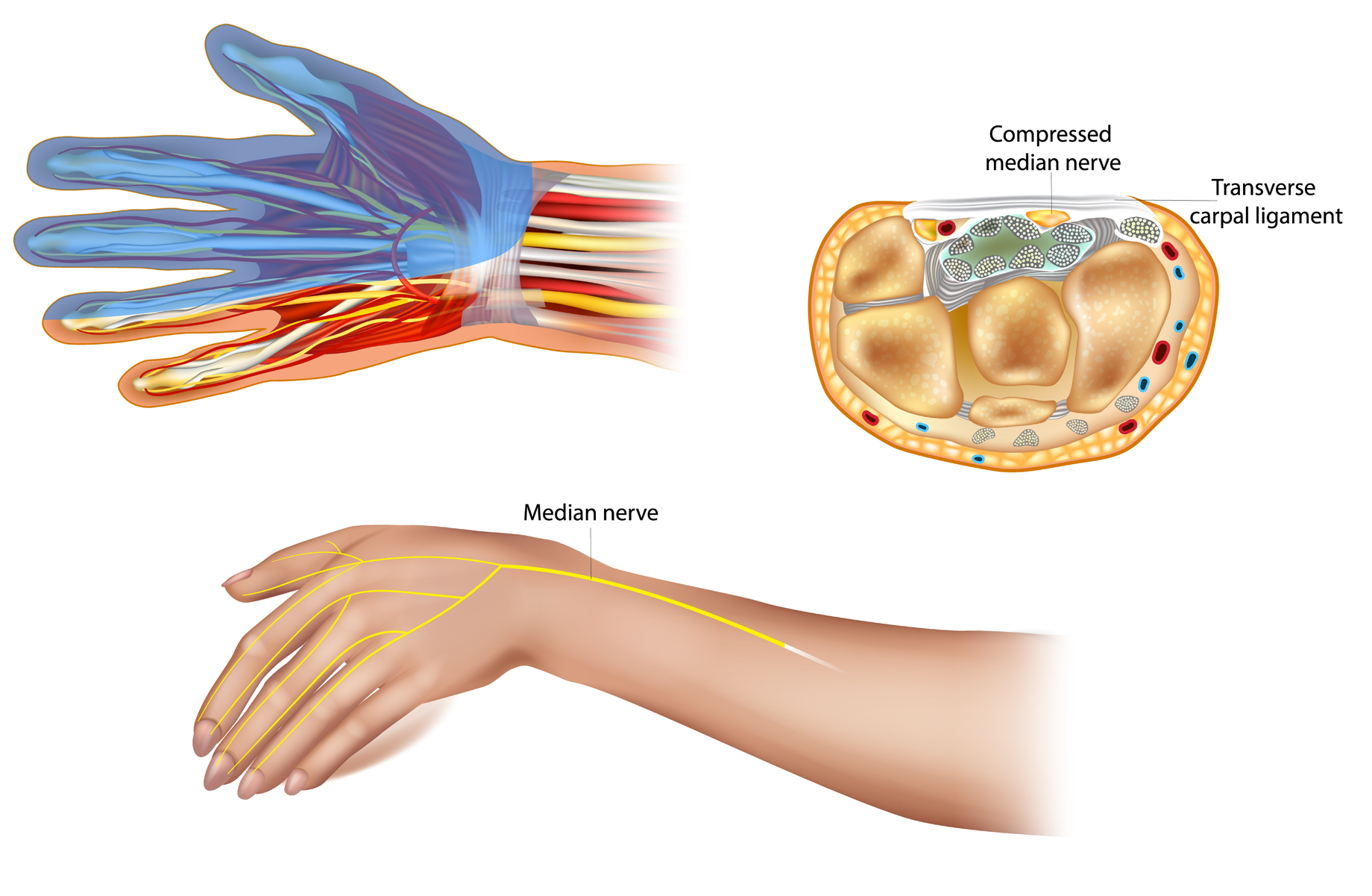
The median nerve travels from the arm to the fingers through the carpal tunnel, providing sensation and motor control to parts of the hand. Inflammation can compress the nerve beneath the transverse carpal ligament at the wrist, leading to pain and functional issues in the hand and arm. Source: Veterans Affairs Canada (2024).
Clinical features
The clinical presentation of carpal tunnel syndrome (CTS) is marked by symptoms affecting the hand and wrist's function and comfort, largely due to compression of the median nerve within the carpal tunnel. Common symptoms include sharp or burning pain, a sensation of the hand 'falling asleep,' or experiencing 'pins and needles,' especially in the thumb, index, middle, and part of the ring fingers. These symptoms often worsen at night or upon waking, largely attributed to the flexed wrist position during sleep, increasing the pressure within the carpal tunnel.
A notable reduction in hand grip strength and challenges in performing precision-required tasks often lead to difficulties in handling objects securely. Advanced stages of CTS may lead to marked atrophy of the muscles of the base of thumb (thenar eminence ), crucial for hand operations.
Diagnostic procedures such as Phalen’s maneuver and Tinel’s sign are instrumental in reinforcing a CTS diagnosis, providing further clinical evidence.
It has been observed that CTS shows a higher prevalence among females, possibly due to anatomical differences such as a comparatively smaller carpal tunnel area. Furthermore, pregnancy has been identified as a significant risk factor for CTS, although the majority of cases tend to resolve within weeks to months post-partum.
Entitlement considerations
In this section
Section A: Causes and/or aggravation
Section B: Medical conditions which are to be included in entitlement/assessment
Section A: Causes and/or aggravation
For VAC entitlement purposes, the following factors are accepted to cause or aggravate the conditions included in the Definition section of this EEG, and may be considered along with the evidence to assist in establishing a relationship to service. The factors have been determined based on a review of up-to-date scientific and medical literature, as well as evidence-based medical best practices. Factors other than those listed may be considered, however consultation with a disability consultant or medical advisor is recommended.
The timelines cited below are for guidance purposes. Each case should be adjudicated on the evidence provided and its own merits.
Factors
- Overuse: Performing any combination of forceful and/or repetitive activities with the affected hand or forearm for an average of at least eight hours per week for a cumulative period of at least six months before the clinical onset of CTS. If specified activities have ceased before the clinical onset or aggravation of CTS, then onset or aggravation must have occurred within 30 days of cessation.
Note: Computer use of 28 hours or more per week may aggravate CTS; however, is not considered causative.
Forceful means applying a substantial amount of force or pressure, using the muscles of the hand or forearm.
Repetitive means performing the same or similar hand or forearm movements repeatedly over time.
Specified activities include:
- Repetitive activities using the affected hand, involving either:
- bending or twisting of the hand or wrist at least 50 times per hour; or
- carrying out the same or similar movements in the hand or wrist at least 50 times per hour.
- Forceful activities generated by the affected hand. This force is applied through:
- equivalent to lifting or carrying loads of more than three kilograms; or
- involving lifting or carrying an object in the hand greater than one kilogram in excess of 10 times per hour.
- Activities where the affected hand or forearm is directly vibrated.
- Activities where the affected hand is used for weight-bearing.
- Activities requiring extended or extreme positions with excess wrist flexion or extension:
- having a flexion/extension angle greater than 45 degrees for a substantial part of the day; or
- ulnar deviation greater than 20 degrees for a substantial part of the day.
Note: Holding an object in grip or pinch position with extreme posture is an exception, and requires that the position be held for most of the day.
- Repetitive activities using the affected hand, involving either:
- Experiencing an injury to the affected wrist, other than a wrist fracture, prior to clinical onset or aggravation of CTS. The injury would have had to:
- alter the normal contour of the carpal tunnel; or
- damage the median nerve or flexor tendons within the carpal tunnel; or
- damage the forearm muscles forming the flexor tendons within the carpal tunnel.
For the injury to cause or aggravate CTS, the symptoms of CTS must commence within several months of the injury.
- Experiencing a fracture to the affected wrist prior to clinical onset or aggravation of CTS. The wrist fracture would alter the normal contour of the carpal tunnel, or damage the median nerve or flexor tendons within the carpal tunnel. For the wrist fracture to cause or aggravate CTS, the symptoms must commence within several months of the fracture.
- Surgery to the affected wrist prior to clinical onset or aggravation of CTS. The surgery would have had to alter the normal contour of the carpal tunnel, or damage the median nerve or flexor tendons within the carpal tunnel. For the surgery to cause or aggravate CTS, symptoms must commence within several months of the surgery.
- Persons with end stage renal disease on hemodialysis prior to clinical onset or aggravation CTS. For hemodialysis to cause or aggravate CTS, it must take place for a period of at least one year immediately before clinical onset or aggravation of CTS. There is no direct evidence that peritoneal dialysis promotes CTS.
- Having diabetes mellitus at the time of clinical onset or aggravation of CTS. People living with diabetic polyneuropathy are at higher risk than diabetics without polyneuropathy.
Note: For diabetes mellitus to cause or aggravate CTS, it must have existed for approximately five years immediately before the clinical onset or aggravation of CTS.
- Having edema involving the affected carpal tunnel at the time of clinical onset or aggravation of CTS. Edema involving the affected carpal tunnel may occur with external burns, fractures, lymphedema, myxedema and animal envenomation.
- Having rheumatoid arthritis involving the affected wrist prior to clinical onset or aggravation of CTS.
- Having gout of the affected wrist prior to clinical onset or aggravation of CTS.
- Having a space occupying lesion of the carpal tunnel prior to clinical onset or aggravation of CTS. The lesion situated within the affected carpal tunnel could include, but is not limited to the following:
- hemangioma
- neuroma of the median nerve
- aneurysm of the median artery
- calcification
- synovial sarcoma
- tendon sheath fibroma
- lipoma and ganglion.
- Pregnancy prior to clinical onset or aggravation of CTS. While pregnancy may cause or aggravate CTS, CTS caused solely from a pregnancy is generally considered reversible within a few months of the completion of the pregnancy.
- Hyperthyroidism, including treated hyperthyroidism, at the time of clinical onset or aggravation of CTS.
- Inability to obtain appropriate clinical management of CTS.
Section B: Medical conditions which are to be included in entitlement/assessment
Section B provides a list of diagnosed medical conditions which are considered for VAC purposes to be included in the entitlement and assessment of carpal tunnel syndrome. No included medical conditions were identified at the time of the publication of this EEG.
Section C: Common medical conditions which may result, in whole or in part, from carpal tunnel syndrome and/or its treatment
No consequential medical conditions were identified at the time of the publication of this EEG. If the merits of the case and medical evidence indicate that a possible consequential relationship may exist, consultation with a disability consultant or medical advisor is recommended.
Links
Related VAC guidance and policy:
- Rheumatoid Arthritis – Entitlement Eligibility Guidelines
- Pain and Suffering Compensation – Policies
- Royal Canadian Mounted Police Disability Pension Claims – Policies
- Establishing the Existence of a Disability – Policies
- Disability Benefits in Respect of Peacetime Military Service – The Compensation Principle – Policies
- Disability Benefits in Respect of Wartime and Special Duty Service – The Insurance Principle – Policies
- Disability Resulting from a Non-Service Related Injury or Disease – Policies
- Consequential Disability – Policies
- Benefit of Doubt – Policies
References as of 22 January 2025
Andersen, J. H., Thomsen, J. F., Overgaard, E., Lassen, C. F., Brandt, L. P. A., Vilstrup, I., Kryger, A. I., & Mikkelsen, S. (2003). Computer Use and Carpal Tunnel Syndrome: A 1-Year Follow-up Study. JAMA, 289(22), 2963. https://doi.org/10.1001/jama.289.22.2963
Anderson, V., Bernard, B., Burt, S. E., Cole, L. L., Estill, C., Fine, L., Grant, K., Gjessing, C., Jenkins, L., Hurrell, J. J., Nelson, N., Pfirman, D., Roberts, R., Stetson, D., Haring-Sweeney, M., & Tanaka, S. (1997). Musculoskeletal Disorders and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back.
Atroshi, I., Gummesson, C., Ornstein, E., Johnsson, R., & Ranstam, J. (2007). Carpal tunnel syndrome and keyboard use at work: A population‐based study. Arthritis & Rheumatism, 56(11), 3620–3625. https://doi.org/10.1002/art.22956
Australian Government Repatriation Medical Authority (2001). Statement of Principles concerning carpal tunnel syndrome (Reasonable Hypothesis) (No. 89 of 2001). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority (2001). Statement of Principles concerning carpal tunnel syndrome (Balance of Probabilities) (No. 90 of 2001). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority (2021). Statement of Principles concerning carpal tunnel syndrome (Balance of Probabilities) (No. 94 of 2021). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority (2021). Statement of Principles concerning carpal tunnel syndrome (Reasonable Hypothesis) (No. 93 of 2021). SOPs - Repatriation Medical Authority
Barcenilla, A., March, L. M., Chen, J. S., & Sambrook, P. N. (2012). Carpal tunnel syndrome and its relationship to occupation: A meta-analysis. Rheumatology, 51(2), 250–261. https://doi.org/10.1093/rheumatology/ker108
Briggs, A. M., Cross, M. J., Hoy, D. G., Sànchez-Riera, L., Blyth, F. M., Woolf, A. D., & March, L. (2016). Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization World Report on Ageing and Health. The Gerontologist, 56(Suppl 2), S243–S255. https://doi.org/10.1093/geront/gnw002
Calandruccio, J. H., & Thompson, N. B. (2018). Carpal Tunnel Syndrome. Orthopedic Clinics of North America, 49(2), 223–229. https://doi.org/10.1016/j.ocl.2017.11.009
Canadian Centre for Occupational Health and Safety. Carpal Tunnel Syndrome. https://www.ccohs.ca/oshanswers/diseases/carpal.html#section-3-hdr
Cazares-Manríquez, M. A., Wilson, C. C., Vardasca, R., García-Alcaraz, J. L., Olguín-Tiznado, J. E., López-Barreras, J. A., & García-Rivera, B. R. (2020). A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex. Applied Sciences, 10(10), 3488. https://doi.org/10.3390/app10103488
Cecil, R. L., Goldman, L., & Bennett, J. C. (Eds.). (2000). Cecil textbook of medicine (21st ed). W.B. Saunders.
Conlon, C. F., & Rempel, D. M. (2005). Upper Extremity Mononeuropathy Among Engineers: Journal of Occupational and Environmental Medicine, 47(12), 1276–1284. https://doi.org/10.1097/01.jom.0000181748.08188.8b
Dale, A. M., Zeringue, A., Harris-Adamson, C., Rempel, D., Bao, S., Thiese, M. S., Merlino, L., Burt, S., Kapellusch, J., Garg, A., Gerr, F., Hegmann, K. T., Eisen, E. A., & Evanoff, B. (2015). General Population Job Exposure Matrix Applied to a Pooled Study of Prevalent Carpal Tunnel Syndrome. American Journal of Epidemiology, 181(6), 431–439. https://doi.org/10.1093/aje/kwu286
Deal, J. B., & Magee, A. J. (2020). Carpal Tunnel Syndrome in Military Aviators. Military Medicine, 185(9–10), e1506–e1509. https://doi.org/10.1093/milmed/usaa077
Demiryurek, B. E., & Aksoy Gündoğdu, A. (2017). Prevalence of carpal tunnel syndrome and its correlation with pain amongst female hairdressers. International Journal of Occupational Medicine and Environmental Health. https://doi.org/10.13075/ijomeh.1896.01068
Dos Santos Bunn, P., De Oliveira Meireles, F., De Souza Sodré, R., Rodrigues, A. I., & Da Silva, E. B. (2021). Risk factors for musculoskeletal injuries in military personnel: A systematic review with meta-analysis. International Archives of Occupational and Environmental Health, 94(6), 1173–1189. https://doi.org/10.1007/s00420-021-01700-3
Eleftheriou, A., Rachiotis, G., Varitimidis, S. E., Koutis, C., Malizos, K. N., & Hadjichristodouloul, C. (2012). Cumulative keyboard strokes: A possible risk factor for carpal tunnel syndrome. Journal of Occupational Medicine and Toxicology, 7(1), 16. https://doi.org/10.1186/1745-6673-7-16
Fagarasanu, M., & Kumar, S. (2003). Carpal tunnel syndrome due to keyboarding and mouse tasks: A review. International Journal of Industrial Ergonomics, 31(2), 119–136. https://doi.org/10.1016/S0169-8141(02)00180-4
Fauci, A. S., Braunwald, E., & Fuselbacher, K. J. (1998). Harrison's principles of internal medicine (14th ed). McGraw Hill.
Garland, F. C., Garland, C. F., Doyle, E. J., Balazs, L. L., Levine, R., Pugh, W. M., & Gorham, E. D. (1996). Carpal Tunnel Syndrome and Occupation in U.S. Navy Enlisted Personnel. Archives of Environmental Health: An International Journal, 51(5), 395–407. https://doi.org/10.1080/00039896.1996.9934428
Genova, A., Dix, O., Saefan, A., Thakur, M., & Hassan, A. (2020). Carpal Tunnel Syndrome: A Review of Literature. Cureus. https://doi.org/10.7759/cureus.7333
Gilliland, B. C. (1994). Relapsing polychondritis and miscellaneous arthritides. Harrison’s principles of internal medicine (pp. 1706-1708): McGraw Hill.
Greathouse, D. G., Root, T. M., Carrillo, C. R., Jordan, C. L., Pickens, B. B., Sutlive, T. G., Shaffer, S. W., & Moore, J. F. (2011). Clinical and electrodiagnostic abnormalities of the median nerve in Army dental assistants before and after training as preventive dental specialists. U.S. Army Medical Department Journal, 70–81.
Haddiya, I., Yacoubi, H., & Bentata, Y. (2018). Why does Carpal Tunnel Syndrome Still Occur in our Chronic Hemodialysis Patients? Journal of Nephrology & Therapeutics, 08(03). https://doi.org/10.4172/2161-0959.1000310
Hagberg, M., Morgenstern, H., & Kelsh, M. (1992). Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scandinavian Journal of Work, Environment & Health, 18(6), 337–345. https://doi.org/10.5271/sjweh.1564
Hagberg, M., Nyström, A., & Zetterlund, B. (1991). Recovery from symptoms after carpal tunnel syndrome surgery in males in relation to vibration exposure. The Journal of Hand Surgery, 16(1), 66–71. https://doi.org/10.1016/S0363-5023(10)80015-2
Harris-Adamson, C., Eisen, E. A., Neophytou, A., Kapellusch, J., Garg, A., Hegmann, K. T., Thiese, M. S., Dale, A. M., Evanoff, B., Bao, S., Silverstein, B., Gerr, F., Burt, S., & Rempel, D. (2016). Biomechanical and psychosocial exposures are independent risk factors for carpal tunnel syndrome: Assessment of confounding using causal diagrams. Occupational and Environmental Medicine, oemed-2016-103634. https://doi.org/10.1136/oemed-2016-103634
Hassan, A., Beumer, A., Kuijer, P. P. F. M., & van der Molen, H. F. (2022). Work‐relatedness of carpal tunnel syndrome: Systematic review including meta‐analysis and GRADE. Health Science Reports, 5(6), e888. https://doi.org/10.1002/hsr2.888
Hatano, M., Kitajima, I., Yamamoto, S., Nakamura, M., Isawa, K., Suwabe, T., Hoshino, J., Sawa, N., & Ubara, Y. (2022). Dialysis-related carpal tunnel syndrome in the past 40 years. Clinical and Experimental Nephrology, 26(1), 68–74. https://doi.org/10.1007/s10157-021-02122-8
Hou, W., Hsu, J., Lin, C., & Liang, H. (2007). Carpal tunnel syndrome in male visual display terminal (VDT) workers. American Journal of Industrial Medicine, 50(1), 1–7. https://doi.org/10.1002/ajim.20396
Jackson, R., Beckman, J., Frederick, M., Musolin, K., & Harrison, R. (2018). Rates of Carpal Tunnel Syndrome in a State Workers’ Compensation Information System, by Industry and Occupation—California, 2007–2014. MMWR. Morbidity and Mortality Weekly Report, 67(39), 1094–1097. https://doi.org/10.15585/mmwr.mm6739a4
Katz, J. N., Larson, M. G., Fossel, A. H., & Liang, M. H. (1991). Validation of a surveillance case definition of carpal tunnel syndrome. American Journal of Public Health, 81(2), 189–193. https://doi.org/10.2105/AJPH.81.2.189
Kothari, M. (2024). Carpal tunnel syndrome: Clinical manifestations and diagnosis. UpToDate.
Kothari, M. (2024). Carpal tunnel syndrome : Pathophysiology and risk factors. UpToDate.
Kozak, A., Schedlbauer, G., Wirth, T., Euler, U., Westermann, C., & Nienhaus, A. (2015). Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: An overview of systematic reviews and a meta-analysis of current research. BMC Musculoskeletal Disorders, 16(1), 231. https://doi.org/10.1186/s12891-015-0685-0
Kuharić, M., & Zibar, L. (2019). Screening for Carpal Tunnel Syndrome in Patients on Chronic Hemodialysis. Acta Medica Academica, 48(2), 167. https://doi.org/10.5644/ama2006-124.255
Lalumandier, J. A., & McPhee, S. D. (2001). Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. Journal of Dental Hygiene: JDH, 75(2), 130–134.
Lalumandier, J. A., McPhee, S. D., Riddle, S., Shulman, J. D., & Daigle, W. W. (2000). Carpal tunnel syndrome: Effect on Army dental personnel. Military Medicine, 165(5), 372–378.
Lawson, I. J. (2020). Is carpal tunnel syndrome caused by work with vibrating tools? Occupational Medicine, 70(1), 8–10. https://doi.org/10.1093/occmed/kqz142
Lin, S., Lin, C., Hsu, W., Lin, C., Lo, S., & Kao, C. (2021). Risk of idiopathic peripheral neuropathy in end‐stage renal disease: A population‐based cohort study. International Journal of Clinical Practice, 75(1). https://doi.org/10.1111/ijcp.13641
Lovalekar, M., Hauret, K., Roy, T., Taylor, K., Blacker, S. D., Newman, P., Yanovich, R., Fleischmann, C., Nindl, B. C., Jones, B., & Canham-Chervak, M. (2021). Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. Journal of Science and Medicine in Sport, 24(10), 963–969. https://doi.org/10.1016/j.jsams.2021.03.016
Lund, C. B., Mikkelsen, S., Thygesen, L. C., Hansson, G.-Å., & Thomsen, J. F. (2019). Movements of the wrist and the risk of carpal tunnel syndrome: A nationwide cohort study using objective exposure measurements. Occupational and Environmental Medicine, 76(8), 519–526. https://doi.org/10.1136/oemed-2018-105619
Maghsoudipour, M., Hosseini, F., Coh, P., & Garib, S. (2021). Evaluation of occupational and non-occupational risk factors associated with carpal tunnel syndrome in dentists. Work, 69(1), 181–186. https://doi.org/10.3233/WOR-213467
Mahoney, J. (1995). Cumulative trauma disorders and carpal tunnel syndrome: Sorting out the confusion. Canadian Journal of Plastic Surgery, 3(4), 17–25. https://doi.org/10.1177/229255039500300404
Mayo Foundation for Medical Education and Research. (2024). Carpal tunnel syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/carpal-tunnel-syndrome/symptoms-causes/syc-20355603
McCarty, D. J. (1979). Arthritis and Allied Conditions: A Textbook of Rheumatology. Lippincott Williams & Wilkins. https://books.google.ca/books?id=jlNsAAAAMAAJ
McDiarmid, M., Oliver, M., Ruser, J., & Gucer, P. (2000). Male and Female Rate Differences in Carpal Tunnel Syndrome Injuries: Personal Attributes or Job Tasks? Environmental Research, 83(1), 23–32. https://doi.org/10.1006/enrs.2000.4042
Mediouni, Z., Bodin, J., Dale, A. M., Herquelot, E., Carton, M., Leclerc, A., Fouquet, N., Dumontier, C., Roquelaure, Y., Evanoff, B. A., & Descatha, A. (2015). Carpal tunnel syndrome and computer exposure at work in two large complementary cohorts. BMJ Open, 5(9), e008156. https://doi.org/10.1136/bmjopen-2015-008156
Mediouni, Z., de Roquemaurel, A., Dumontier, C., Becour, B., Garrabe, H., Roquelaure, Y., & Descatha, A. (2014). Is Carpal Tunnel Syndrome Related to Computer Exposure at Work? A Review and Meta-Analysis. Journal of Occupational & Environmental Medicine, 56(2), 204–208. https://doi.org/10.1097/JOM.0000000000000080
Miyasaka, N., Sato, K., Kitano, Y., Higaki, M., Nishioka, K., & Ohta, K. (1992). Aberrant cytokine production from tenosynovium in dialysis associated amyloidosis. Annals of the Rheumatic Diseases, 51(6), 797–802. https://doi.org/10.1136/ard.51.6.797
Nathan, P. A., Keniston, R. C., Myers, L. D., & Meadows, K. D. (1992). Obesity as a risk factor for slowing of sensory conduction of the median nerve in industry. A cross-sectional and longitudinal study involving 429 workers. Journal of Occupational Medicine.: Official Publication of the Industrial Medical Association, 34(4), 379–383.
Neuroscience Specialists. (2022, January 27). Does consistent typing cause carpal tunnel?. https://www.neurosurg.org/blog/does-consistent-typing-cause-carpal-tunnel/?bp=29218
Newington, L., Harris, E. C., & Walker-Bone, K. (2015). Carpal tunnel syndrome and work. Best Practice & Research Clinical Rheumatology, 29(3), 440–453. https://doi.org/10.1016/j.berh.2015.04.026
Niu, S. (2022). Diagnostic and Exposure Criteria for Occupational Diseases: Guidance Notes for Diagnosis and Prevention of the Diseases in the ILO List of Occupational Diseases (revised 2010) (C. Colosio, Ed.). International Labour Organisation.
O’Leary, T. J., Young, C. D., Wardle, S. L., & Greeves, J. P. (2023). Gender data gap in military research: A review of the participation of men and women in military musculoskeletal injury studies. BMJ Military Health, 169(1), 84–88. https://doi.org/10.1136/bmjmilitary-2021-002015
Padua, L., Cuccagna, C., Giovannini, S., Coraci, D., Pelosi, L., Loreti, C., Bernabei, R., & Hobson-Webb, L. D. (2023). Carpal tunnel syndrome: Updated evidence and new questions. The Lancet Neurology, 22(3), 255–267. https://doi.org/10.1016/S1474-4422(22)00432-X
Phalen, G. S. (1966). The carpal-tunnel syndrome. Seventeen years’ experience in diagnosis and treatment of six hundred fifty-four hands. The Journal of Bone and Joint Surgery. American Volume, 48(2), 211–228.
Pisquiy, J. J., Chan, A. G., Prabhakar, G., Kusnezov, N., & Dunn, J. C. (2019). Incidence of Cubital Tunnel Syndrome in the U.S. Military Population. The Journal of Hand Surgery, 44(6), 516.e1-516.e7. https://doi.org/10.1016/j.jhsa.2018.08.003
Radecki, P. (1994). The familial occurrence of carpal tunnel syndrome. Muscle & Nerve, 17(3), 325–330. https://doi.org/10.1002/mus.880170311
Rajczewski, A., Daroszewski, P., Fabijański, A., Bogusławski, K., Kaźmierczak, M., & Huber, J. (2023). Incidence of Carpal Tunnel Syndrome and Other Coexisting Brachial Plexus Neuropathies in Bullseye Shooters—A Pilot Retrospective Clinical and Neurophysiological Assessment. Applied Sciences, 13(14), 8020. https://doi.org/10.3390/app13148020
Raman, S. R., Al-Halabi, B., Hamdan, E., & Landry, M. D. (2012). Prevalence and risk factors associated with self-reported carpal tunnel syndrome (CTS) among office workers in Kuwait. BMC Research Notes, 5(1), 289. https://doi.org/10.1186/1756-0500-5-289
Rempel, D. M., Keir, P. J., & Bach, J. M. (2008). Effect of wrist posture on carpal tunnel pressure while typing. Journal of Orthopaedic Research, 26(9), 1269–1273. https://doi.org/10.1002/jor.20599
Rhon, D. l I., Molloy, J. M., Monnier, A., Hando, B. R., & Newman, P. M. (2022). Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta-analysis. European Journal of Sport Science, 22(1), 16–34.https://doi.org/10.1080/17461391.2021.1931464
Rigouin, P., Ha, C., Bodin, J., Le Manac’h, A. P., Descatha, A., Goldberg, M., & Roquelaure, Y. (2014). Organizational and psychosocial risk factors for carpal tunnel syndrome: A cross-sectional study of French workers. International Archives of Occupational and Environmental Health, 87(2), 147–154. https://doi.org/10.1007/s00420-013-0846-0
Roquer, J., & Cano, J. F. (2009). Carpal tunnel syndrome and hyperthyroidism: A prospective study. Acta Neurologica Scandinavica, 88(2), 149–152. https://doi.org/10.1111/j.1600-0404.1993.tb04207.x
Rosenstock, L., & Cullen, M. R. (Eds.). (1994). Textbook of clinical occupational and environmental medicine. Saunders.
Rosenstock, L. (2005). Textbook of Clinical Occupational and Environmental Medicine. Elsevier Saunders. https://books.google.ca/books?id=gRtnQgAACAAJ
Ruddy, S., Harris, E. D., Sledge, C. B., & Kelley, W. N. (2001). Kelley’s textbook of rheumatology (6th ed). W.B. Saunders Co. Philadelphia; WorldCat.
Rudzki, W., Delaney, T., & Macri, E. (2017). Military Personnel. In Brukner & Khan’s Clinical Sports Medicine: Injuries (5e ed., Vol. 1–1, pp. 991–1001). McGraw Hill. https://csm.mhmedical.com/content.aspx?bookid=1970§ionid=168697060
Saint-Lary, O., Rébois, A., Mediouni, Z., & Descatha, A. (2015). Carpal Tunnel Syndrome: Primary Care and Occupational Factors. Frontiers in Medicine, 2. https://doi.org/10.3389/fmed.2015.00028
Sammito, S., Hadzic, V., Karakolis, T., Kelly, K. R., Proctor, S. P., Stepens, A., White, G., & Zimmermann, W. O. (2021). Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Military Medical Research, 8(1), 66. https://doi.org/10.1186/s40779-021-00357-w
Samuel L.. Turek, Stuart L.. Weinstein, Buckwalter, J. A., & Turek, S. L. (1994). Turek's Orthopaedics: Principles and Their Application. Lippincott.
Sauni, R., Pääkkönen, R., Virtema, P., Jäntti, V., Kähönen, M., Toppila, E., Pyykkö, I., & Uitti, J. (2009). Vibration-induced white finger syndrome and carpal tunnel syndrome among Finnish metal workers. International Archives of Occupational and Environmental Health, 82(4), 445–453. https://doi.org/10.1007/s00420-008-0357-6
Schwarz, A., Keller, F., Seyfert, S., Pöll, W., Molzahn, M., & Distler, A. (1984). Carpal tunnel syndrome: A major complication in long-term hemodialysis patients. Clinical Nephrology, 22(3), 133–137.
Shaffer, S. W., Koreerat, N. R., Gordon, L. B., Santillo, D. R., Moore, J. H., & Greathouse, D. G. (2013). Median and ulnar neuropathies in U.S. Army Medical Command Band members. Medical Problems of Performing Artists, 28(4), 188–194.
Shiri, R., & Falah-Hassani, K. (2015). Computer use and carpal tunnel syndrome: A meta-analysis. Journal of the Neurological Sciences, 349(1–2), 15–19. https://doi.org/10.1016/j.jns.2014.12.037
Sivri, A., Çeliker, R., Sungur, C., & Kutsal, Y. G. (1994). Carpal Tunnel Syndrome: A Major Complication in Hemodialysis Patients. Scandinavian Journal of Rheumatology, 23(5), 287–290. https://doi.org/10.3109/03009749409103731
Sluiter, J. K., Rest, K. M., & Frings-Dresen, M. H. (2001). Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scandinavian Journal of Work, Environment & Health, 27, 1–102. JSTOR.
Stjernbrandt, A., Vihlborg, P., Wahlström, V., Wahlström, J., & Lewis, C. (2022). Occupational cold exposure and symptoms of carpal tunnel syndrome – a population-based study. BMC Musculoskeletal Disorders, 23(1), 596. https://doi.org/10.1186/s12891-022-05555-8
Stock, S. R. (1991). Workplace ergonomic factors and the development of musculoskeletal disorders of the neck and upper limbs: A meta-analysis. American Journal of Industrial Medicine, 19(1), 87–107. https://doi.org/10.1002/ajim.4700190111
Strasberg, S. R., Novak, C. B., Mackinnon, S. E., & Murray, J. F. (1994). Subjective and employment outcome following secondary carpal tunnel surgery. Annals of Plastic Surgery, 32(5), 485–489. https://doi.org/10.1097/00000637-199405000-00008
Tonga, F., & Bahadir, S. (2022). The Factors Associated with Carpal Tunnel Syndrome Severity. Turkish Neurosurgery, 32(3), 392–397. https://doi.org/10.5137/1019-5149.JTN.34519-21.2
Toosi, K. K., Hogaboom, N. S., Oyster, M. L., & Boninger, M. L. (2015). Computer keyboarding biomechanics and acute changes in median nerve indicative of carpal tunnel syndrome. Clinical Biomechanics, 30(6), 546–550. https://doi.org/10.1016/j.clinbiomech.2015.04.008
Tsai, C.-H., Hsu, H.-H., Chen, S.-H., Chien, L., Lin, J. A.-J., Chang, C.-J., & Kao, H.-K. (2020). Incidence and Risk of Carpal Tunnel Syndrome in End-Stage Renal Disease Patients on Dialysis: A Nationwide Population-Based Matched Cohort Study. Annals of Plastic Surgery, 84(1S Suppl 1), S100–S106. https://doi.org/10.1097/SAP.0000000000002181
Veterans Affairs Canada (2024). Carpal Tunnel Syndrome. License purchased for use from https://www.123rf.com/photo_180510408_carpal-tunnel-syndrome-compressed-median-nerve-anatomy-of-the-carpal-tunnel-showing-the-median.html
Wijnhoven, H. A. H., De Vet, H. C. W., & Picavet, H. S. J. (2006). Prevalence of musculoskeletal disorders is systematically higher in women than in men. The Clinical Journal of Pain, 22(8), 717–724. https://doi.org/10.1097/01.ajp.0000210912.95664.53
Wolf, J. M., Mountcastle, S., & Owens, B. D. (2009). Incidence of carpal tunnel syndrome in the US military population. Hand (New York, N.Y.), 4(3), 289–293. https://doi.org/10.1007/s11552-009-9166-y
Woo, E. H. C., White, P., & Lai, C. W. K. (2019). Morphological Changes of the Median Nerve Within the Carpal Tunnel During Various Finger and Wrist Positions: An Analysis of Intensive and Nonintensive Electronic Device Users. The Journal of Hand Surgery, 44(7), 610.e1-610.e15. 5https://doi.org/10.1016/j.jhsa.2018.08.006
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/