Entitlement Eligibility Guideline (EEG)
Date reviewed: 22 January 2025
Date created: February 2005
ICD-11 codes: NC96.0, FB50
VAC medical codes:
72670
Achilles tendonitis, ruptured Achilles tendon
01328
Chronic Achilles bursitis
This publication is available upon request in alternate formats.
Full document – PDF Version
Definition
Chronic Achilles tendon conditions are characterized by pain, swelling, and diminished performance of the tendon. For the purposes of this entitlement eligibility guideline (EEG), chronic Achilles tendon conditions include:
- chronic Achilles tendinopathy
- chronic Achilles tendinosis/tendonitis
- chronic Achilles bursitis
- Achilles tendon tear or rupture
Diagnostic standard
Diagnosis by a qualified physician (orthopedic surgeon, family physician), nurse practitioner, or physician assistant (within their scope of practice) is required.
Confirmation of chronic Achilles tendonitis and Achilles bursitis may involve investigations such as ultrasound or magnetic resonance imaging (MRI) to evaluate the structural integrity and inflammation of the Achilles tendon and surrounding bursa.
Anatomy and physiology
The Achilles tendon and associated bursae work together to enable essential activities such as standing on tiptoe and propelling the body forward during walking or running.
Achilles tendinopathy is an umbrella term that describes a broad range of Achilles tendon conditions characterized by pain, functional impairment, and often structural changes within the tendon that connects the gastrocnemius muscle (calf) to the calcaneus (heel bone).
Achilles tendinosis refers to degenerative changes in the Achilles tendon characterized by abnormal tissue regeneration, disorganized collagen fibers, and a lack of inflammatory cells (Figure 1: Conditions of the Achilles tendon).
Achilles tendonitis and Achilles bursitis are conditions that involve the Achilles tendon and its surrounding structures, which are essential for foot movement and stability. The Achilles tendon, the largest and strongest tendon in the body, connects the gastrocnemius muscle (calf) to the heel bone (calcaneus), enabling walking, running, and jumping activities. This tendon works by transmitting the force generated by the calf muscles to the foot, providing the necessary leverage for movement. The retrocalcaneal bursa, situated between the Achilles tendon and the heel bone, allows for smooth movement of the Achilles tendon over the heel bone.
In chronic Achilles tendonitis, the tendon itself becomes chronically inflamed, often due to overuse, leading to pain, swelling, and decreased function. Injury or recurrent stress can result in microtears, inflammation, and subsequent degeneration.
Chronic Achilles bursitis involves chronic inflammation of the bursa adjacent to the tendon, which can also result from overuse or direct injury. This inflammation can exacerbate or mimic the symptoms of Achilles tendonitis.
Achilles tendon rupture involves the complete or partial tear of the Achilles tendon. This can result from chronic degeneration or from a traumatic force.
Figure 1: Conditions of the Achilles tendon
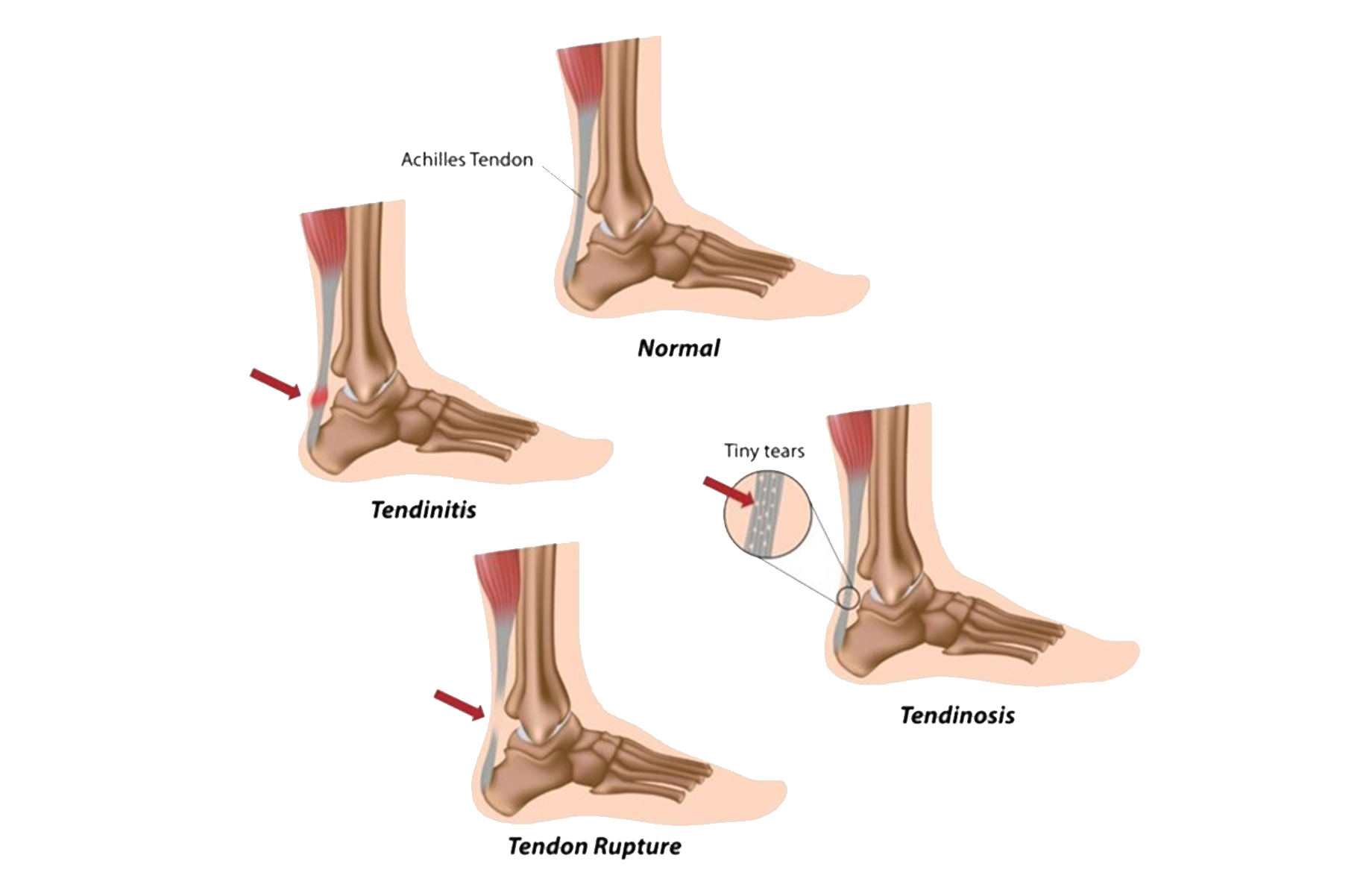
An Achilles tendon injury can be classified into three main types: tendinitis (inflammation due to overuse), tendinosis (degeneration with tiny tears in the tendon), and tendon rupture (a tear often caused by sudden trauma). Source: Veterans Affairs Canada (2024).
Clinical features
The clinical presentation of chronic Achilles tendonitis and Achilles bursitis is marked by chronic pain at the back of the heel, which can extend up the tendon towards the calf. This pain is often described as a sharp or burning sensation that intensifies with physical activity, particularly running or jumping, and may improve with rest. Morning stiffness and pain are common, with individuals noting a significant discomfort upon taking the first steps after waking.
Swelling along the tendon or at the back of the heel signifies inflammation and may be accompanied by redness and warmth to the touch. In cases of Achilles bursitis, the swelling is more localized to the area of the bursa, just above where the heel bone meets the Achilles tendon.
Functionally, those affected may experience difficulty in performing activities that require pushing off with the foot, such as climbing stairs or standing on tiptoe. The range of motion in the ankle may be reduced, particularly in dorsiflexion (pulling the foot up towards the shin), due to pain and stiffness in the Achilles tendon.
Chronic or severe cases of Achilles tendonitis can lead to degenerative changes within the tendon, known as tendinosis, characterized by thickening of the tendon, nodules, and increased risk of tendon rupture. Similarly, persistent inflammation in Achilles bursitis causes chronic discomfort and can impact the function of the foot and ankle.
Female service members have a significantly lower risk of Achilles tendinopathy compared to their male counterparts. Female sex is a protective factor in the administrative and logistic enlisted specialties however, enlisted female members have a higher risk for Achilles tendinopathy in the maintenance and naval specialties.
Entitlement considerations
In this section
Section A: Causes and/or aggravation
Section B: Medical conditions which are to be included in entitlement/assessment
Section A: Causes and/or aggravation
For Veterans Affairs Canada (VAC) entitlement purposes, the following factors are accepted to cause or aggravate the conditions included in the Definition section of this EEG, and may be considered along with the evidence to assist in establishing a relationship to service. The factors have been determined based on a review of up-to-date scientific and medical literature, as well as evidence-based medical best practices. Factors other than those listed may be considered, however consultation with a disability consultant or medical advisor is recommended.
The timelines cited below are for guidance purposes. Each case should be adjudicated on the evidence provided and its own merits.
Factors
- Overuse prior to the clinical onset or aggravation of an Achilles tendon condition.
Note: Clinical manifestations of an Achilles condition should occur during the activity or within seven days of its cessation and be ongoing or recurrent for at least six months.
- Preexisting or concurrent conditions:
- Having a prior lower limb fracture resulting in an altered alignment, at the time of clinical onset or aggravation of an Achilles tendon condition.
- Having one or more of the following systemic arthritic diseases at the time of clinical onset or aggravation of Achilles tendinopathy or bursitis:
- ankylosing spondylitis
- Behcet syndrome
- gout or another crystal-induced arthropathy
- enteropathic spondyloarthropathy
- psoriatic arthropathy
- reactive arthritis
- rheumatoid arthritis
- undifferentiated spondyloarthropathy.
Note: Where a chronic Achillies tendinopathy or bursitis is part of the symptomatology of another condition, it is included in the entitlement and assessment of that condition.
- For Achilles tendinopathy only, being treated with a fluoroquinolone antibiotic (including, but not limited to, levofloxacin and ciprofloxacin), within seven days before clinical onset or aggravation of Achilles tendinopathy.
- Being treated with a systemic glucocorticoid medication for a duration of at least six months before the clinical onset or aggravation of Achilles tendinopathy or bursitis. This factor does not apply to inhaled or topical glucocorticoid medications.
- For Achilles tendinopathy only, being treated with a statin medication, (including, but not limited to, atorvastatin and rosuvastatin), before the clinical onset or aggravation of Achilles tendinopathy.
- Inability to obtain appropriate clinical management of an Achilles tendon condition.
Section B: Medical conditions which are to be included in entitlement/assessment
Section B provides a list of diagnosed medical conditions which are considered for VAC purposes to be included in the entitlement and assessment of chronic Achilles tendon conditions.
- Superficial calcaneal bursitis
- Deep retrocalcaneal bursitis
- Achilles peritendonitis
- Posterior heel adventitial bursitis
- Haglund's syndrome and Haglund's deformity (pump bump)
Section C: Common medical conditions which may result, in whole or in part, from chronic Achilles tendon conditions and/or their treatment
No consequential medical conditions were identified at the time of the publication of this EEG. If the merits of the case and medical evidence indicate that a possible consequential relationship may exist, consultation with a disability consultant or medical advisor is recommended.
Links
Related VAC guidance and policy:
- Ankylosing Spondylitis – Entitlement Eligibility Guidelines
- Rheumatoid Arthritis – Entitlement Eligibility Guidelines
- Pain and Suffering Compensation – Policies
- Royal Canadian Mounted Police Disability Pension Claims – Policies
- Dual Entitlement – Disability Benefits – Policies
- Establishing the Existence of a Disability – Policies
- Disability Benefits in Respect of Peacetime Military Service – The Compensation Principle – Policies
- Disability Benefits in Respect of Wartime and Special Duty Service – The Insurance Principle – Policies
- Disability Resulting from a Non-Service Related Injury or Disease – Policies
- Consequential Disability – Policies
- Benefit of Doubt – Policies
References as of 22 January 2025
Australian Government, Repatriation Medical Authority (1996). Statement of principles concerning Achilles tendinopathy and bursitis (Reasonable Hypothesis) (No 53 of 1996). SOPs - Repatriation Medical Authority
Australian Government, Repatriation Medical Authority (1996). Statement of principles concerning adjustment disorder (Balance of Probabilities) (no. 54 of 1996). SOPs - Repatriation Medical Authority
Australian Government, Repatriation Medical Authority. (2015). Statement of principles concerning Achilles tendinopathy and bursitis (reasonable hypothesis) (No 96 of 2015). SOPs - Repatriation Medical Authority
Australian Government, Repatriation Medical Authority (2015). Statement of principles concerning adjustment disorder (balance of probabilities) (no. 97 of 2015). SOPs - Repatriation Medical Authority
Briggs, A. M., Cross, M. J., Hoy, D. G., Sànchez-Riera, L., Blyth, F. M., Woolf, A. D., & March, L. (2016). Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization World Report on Ageing and Health. The Gerontologist, 56(Suppl 2), S243–S255. https://doi.org/10.1093/geront/gnw002
Canosa-Carro, L., Bravo-Aguilar, M., Abuín-Porras, V., Almazán-Polo, J., García-Pérez-de-Sevilla, G., Rodríguez-Costa, I., López-López, D., Navarro-Flores, E., & Romero-Morales, C. (2022). Current understanding of the diagnosis and management of the tendinopathy: An update from the lab to the clinical practice. Disease-a-Month, 68(10), 101314. https://doi.org/10.1016/j.disamonth.2021.101314
Dee, R. (Ed.). (1997). Principles of orthopaedic practice (2nd ed.). McGraw-Hill, Health Professions Division.
Dos Santos Bunn, P., De Oliveira Meireles, F., De Souza Sodré, R., Rodrigues, A. I., & Da Silva, E. B. (2021). Risk factors for musculoskeletal injuries in military personnel: A systematic review with meta-analysis. International Archives of Occupational and Environmental Health, 94(6), 1173–1189. https://doi.org/10.1007/s00420-021-01700-3
Fauci, A. S., Braunwald, E., & Fuselbacher, K. J. (1998). Harrison's principles of internal medicine (14th ed.). McGraw Hill.
Fraser, J. J., Zellers, J. A., Sullivan, C. K., & Janney, C. F. (2023). Burden and risk factors for Achilles tendon rupture in the military population from 2006 to 2015: A retrospective cohort study [Preprint]. Sports Medicine. https://doi.org/10.1101/2023.10.02.23296425
Harries, M., Williams, C., Stanish, W., & Micheli, L. (1998). Oxford textbook of sports medicine (2nd ed.). Oxford University Press.
Jahss, M. H. (1982). Disorders of the foot. W.B. Saunders.
Järvinen, T. A. H., Kannus, P., Maffulli, N., & Khan, K. M. (2005). Achilles Tendon Disorders: Etiology and Epidemiology. Foot and Ankle Clinics, 10(2), 255–266. https://doi.org/10.1016/j.fcl.2005.01.013
Kibler, W. B., Herring, S. A., & Press, J. M. (1998). Functional rehabilitation of sports and musculoskeletal injuries. Aspen publ.
Kozlovskaia, M., Vlahovich, N., Ashton, K. J., & Hughes, D. C. (2017). Biomedical Risk Factors of Achilles Tendinopathy in Physically Active People: A Systematic Review. Sports Medicine - Open, 3(1), 20. https://doi.org/10.1186/s40798-017-0087-y
Lausé, G. E., Egbert, R. A., & Ryan, P. M. (2023). Insertional Achilles Tendinopathy: Occupational Outcomes in the Military. Foot & Ankle Specialist, 16(4), 342–348. https://doi.org/10.1177/19386400211029121
Lause, G., Egbert, R., Anderson, C., & Ryan, P. (2018). Outcomes of Insertional Achilles Tendinopathy in Active Duty Military Population. Foot & Ankle Orthopaedics, 3(3), 2473011418S0030. https://doi.org/10.1177/2473011418S00304
Lovalekar, M., Hauret, K., Roy, T., Taylor, K., Blacker, S. D., Newman, P., Yanovich, R., Fleischmann, C., Nindl, B. C., Jones, B., & Canham-Chervak, M. (2021). Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. Journal of Science and Medicine in Sport, 24(10), 963–969. https://doi.org/10.1016/j.jsams.2021.03.016
Mahieu, N., Van Tiggelen, D., De Muynck, M., Dumalin, M., & Witvrouw, E. (2010). Blood Flow of the Achilles Tendon During Military Training. International Journal of Sports Medicine, 31(12), 901–905. https://doi.org/10.1055/s-0030-1267159
Maughan, K., Fields, K., & Reid Boggess, B. (2024). Achilles tendinopathy and tendon rupture. UpToDate.
McAuliffe, S., Tabuena, A., McCreesh, K., O’Keeffe, M., Hurley, J., Comyns, T., Purtill, H., O’Neill, S., & O’Sullivan, K. (2019). Altered Strength Profile in Achilles Tendinopathy: A Systematic Review and Meta-Analysis. Journal of Athletic Training, 54(8), 889–900. https://doi.org/10.4085/1062-6050-43-18
Milgrom, C., Finestone, A., Zin, D., Mandel, D., & Novack, V. (2003). Cold Weather Training: A Risk Factor for Achilles Paratendinitis among Recruits. Foot & Ankle International, 24(5), 398–401. https://doi.org/10.1177/107110070302400504
Millar, N. L., Silbernagel, K. G., Thorborg, K., Kirwan, P. D., Galatz, L. M., Abrams, G. D., Murrell, G. A. C., McInnes, I. B., & Rodeo, S. A. (2021). Tendinopathy. Nature Reviews Disease Primers, 7(1), 1. https://doi.org/10.1038/s41572-020-00234-1
O’Leary, T. J., Young, C. D., Wardle, S. L., & Greeves, J. P. (2023). Gender data gap in military research: A review of the participation of men and women in military musculoskeletal injury studies. BMJ Military Health, 169(1), 84–88. https://doi.org/10.1136/bmjmilitary-2021-002015
Owens, B. D., Wolf, J. M., Seelig, A. D., Jacobson, I. G., Boyko, E. J., Smith, B., Ryan, M. A. K., Gackstetter, G. D., Smith, T. C., for the Millennium Cohort Study Team, Bagnell, M., Creaven, G., Crum-Cianflone, N., Davies, J., Granado, N., Hernando, D., Horton, J., Jones, K., LeardMann, C., … Wong, C. (2013). Risk Factors for Lower Extremity Tendinopathies in Military Personnel. Orthopaedic Journal of Sports Medicine, 1(1), 232596711349270. https://doi.org/10.1177/2325967113492707
Purdam, C., & de Vos, R.-J. (2024). Tendinopathy. UpToDate.
Rhon, D. l I., Molloy, J. M., Monnier, A., Hando, B. R., & Newman, P. M. (2022). Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta-analysis. European Journal of Sport Science, 22(1), 16–34. https://doi.org/10.1080/17461391.2021.1931464
Rudzki, W., Delaney, T., & Macri, E. (2017). Military Personnel. In Brukner & Khan’s Clinical Sports Medicine: Injuries (5e ed., Vol. 1–1, pp. 991–1001). McGraw Hill. https://csm.mhmedical.com/content.aspx?bookid=1970§ionid=168697060
Sammito, S., Hadzic, V., Karakolis, T., Kelly, K. R., Proctor, S. P., Stepens, A., White, G., & Zimmermann, W. O. (2021). Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Military Medical Research, 8(1), 66. https://doi.org/10.1186/s40779-021-00357-w
Sellon, E., Goodall, D., Barker-Davies, R., Crick, A., & Ashburner, A. (2020). Musculoskeletal Overuse Injuries of Lower Limb in Military. In K. M. Iyer & W. S. Khan (Eds.), Orthopedics of the Upper and Lower Limb (pp. 635–653). Springer International Publishing. https://doi.org/10.1007/978-3-030-43286-7_36
Steinberg, N., Pantanowitz, M., Zeev, A., Svorai Band, S., Funk, S., & Nemet, D. (2022). Achilles and patellar tendon structure following a prevention program in male combat soldiers. The Physician and Sportsmedicine, 50(6), 531–540. https://doi.org/10.1080/00913847.2021.1976601
Stephenson, M. (2015). Causation and risk factors of Achilles Tendinopathy.
Subotnick, S. I. (Ed.). (1999). Sports medicine of the lower extremity (Ed. 2). Churchill Livingston.
Sullivan, C. K., Janney, C. F., & Fraser, J. J. (2023). Burden and risk factors for Achilles tendinopathy in the military population from 2006 to 2015. A retrospective cohort study. Sports Medicine. https://doi.org/10.1101/2023.02.27.23286521
van der Vlist, A. C., Breda, S. J., Oei, E. H. G., Verhaar, J. A. N., & de Vos, R.-J. (2019). Clinical risk factors for Achilles tendinopathy: A systematic review. British Journal of Sports Medicine, 53(21), 1352–1361. https://doi.org/10.1136/bjsports-2018-099991
Veterans Affairs Canada (2024). Conditions of the Achilles Tendon. License for use purchased from https://www.123rf.com/photo_11347639_Achilles-tendon-problems.html
Weinstein, S. L., Buckwalter, J. A., & Turek, S. L. (Eds.). (1994). Turek’s Orthopaedics: Principles and their application (5th ed). Lippincott.
Wijnhoven, H. A. H., De Vet, H. C. W., & Picavet, H. S. J. (2006). Prevalence of musculoskeletal disorders is systematically higher in women than in men. The Clinical Journal of Pain, 22(8), 717–724. https://doi.org/10.1097/01.ajp.0000210912.95664.53
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/