Entitlement Eligibility Guideline (EEG)
Date reviewed: 22 January 2025
Date created: February 2005
ICD-11 codes: FB55.1, FB55.0
VAC medical code: 72632 Epicondylitis
This publication is available upon request in alternate formats.
Full document – PDF Version
Definition
Chronic elbow tendinopathy encompasses conditions affecting the tendons that attach to the elbow's lateral and medial epicondyles.
For the purposes of this entitlement eligibility guideline (EEG), the following conditions are included:
- chronic elbow tendinopathy
- chronic elbow tendinosis/tendinitis
- chronic elbow epicondylitis (lateral or medial).
Diagnostic standard
Diagnosis by a qualified medical physician (orthopedic surgeon, family physician), nurse practitioner, or physician assistant (within their scope of practice) is required.
The diagnosis is primarily clinical, based on the patient's history of chronic elbow pain, physical examination findings of tenderness at the lateral or medial epicondyle, and pain or weakness with resisted wrist extension or flexion.
Note: For Veterans Affairs Canada (VAC) entitlement purposes, the lateral or medial location of the tendinopathy must be specified.
Anatomy and physiology
Tendinopathy is an umbrella term that describes a broad range of tendon conditions characterized by pain, functional impairment, and often structural changes within the tendons.
Tendinosis refers to degenerative changes in the tendon characterized by abnormal tissue regeneration, disorganized collagen fibers, and a lack of inflammatory cells.
Tendinitis refers to inflammatory changes in the tendons.
Chronic elbow tendinopathy encompasses conditions affecting the tendons that attach to the elbow's lateral and medial epicondyles, giving rise to two distinct forms. Lateral epicondylitis (tennis elbow) and medial epicondylitis (golfer's elbow), are conditions resulting from chronic inflammation at the origin of the elbow extensor and flexor tendons resulting in pain and tenderness.
Lateral epicondylitis (tennis elbow)
The lateral epicondyle anchors the extensor tendons that facilitate wrist extension, which is movement of the hand away from the palm. Lateral epicondylitis is marked by pain and tenderness over the lateral epicondyle of the elbow, the aspect of the elbow which points upward when the palm is flat on a surface. This condition primarily arises from repetitive wrist extension, like the backhand in tennis, or radial deviation movements, leading to microtears and degeneration in the tendon attachment.
Medial epicondylitis (golfer's elbow)
The medial epicondyle anchors the flexor tendons that facilitate wrist flexion, which is movement of the hand toward the palm. Medial epicondylitis is marked by pain and tenderness over the medial epicondyle of the elbow, the aspect of the elbow which points downward when the palm is flat on a surface. Similar to its lateral counterpart, it results from overuse or repetitive forceful wrist flexion and pronation leading to microtears and degeneration in the tendon attachment.
Both conditions manifest as a consequence of overuse or stress, triggering degenerative changes at the tendon origins. Such pathological alterations include structural disorganization and a departure from the normal tendon architecture, directly impacting the elbow's function by inducing pain and limiting movement.
Clinical features
Chronic elbow tendinopathy, either lateral epicondylitis (tennis elbow) and medial epicondylitis (golfer's elbow), exhibits distinctive clinical features corresponding to the affected tendon and the specific movements. The diagnosis is primarily clinical, based on the patient's history of chronic elbow pain, physical examination findings of tenderness at the lateral or medial epicondyle, and pain or weakness with resisted wrist extension or flexion.
Lateral epicondylitis (tennis elbow)
Individuals experiencing tennis elbow commonly describe a progressive onset of pain located at the elbow's lateral aspect (the side of the elbow that faces away when the palm is oriented upwards), potentially extending into the forearm (Figure 1: Lateral epicondylitis). This discomfort is primarily made worse by movements that involve wrist extension (movement of the hand upwards, away from the palm side) or radial deviation (movement of the wrist towards the thumb side). Examples of activities that may provoke symptoms include manipulating a doorknob, executing a backhand stroke in tennis, or lifting objects with the palm facing downwards. This condition is denoted by tenderness at the lateral epicondyle and potentially a reduction in grip strength. The discomfort increases during activities that challenge the wrist to extend against resistance.
Figure 1: Lateral epicondylitis (tennis elbow)
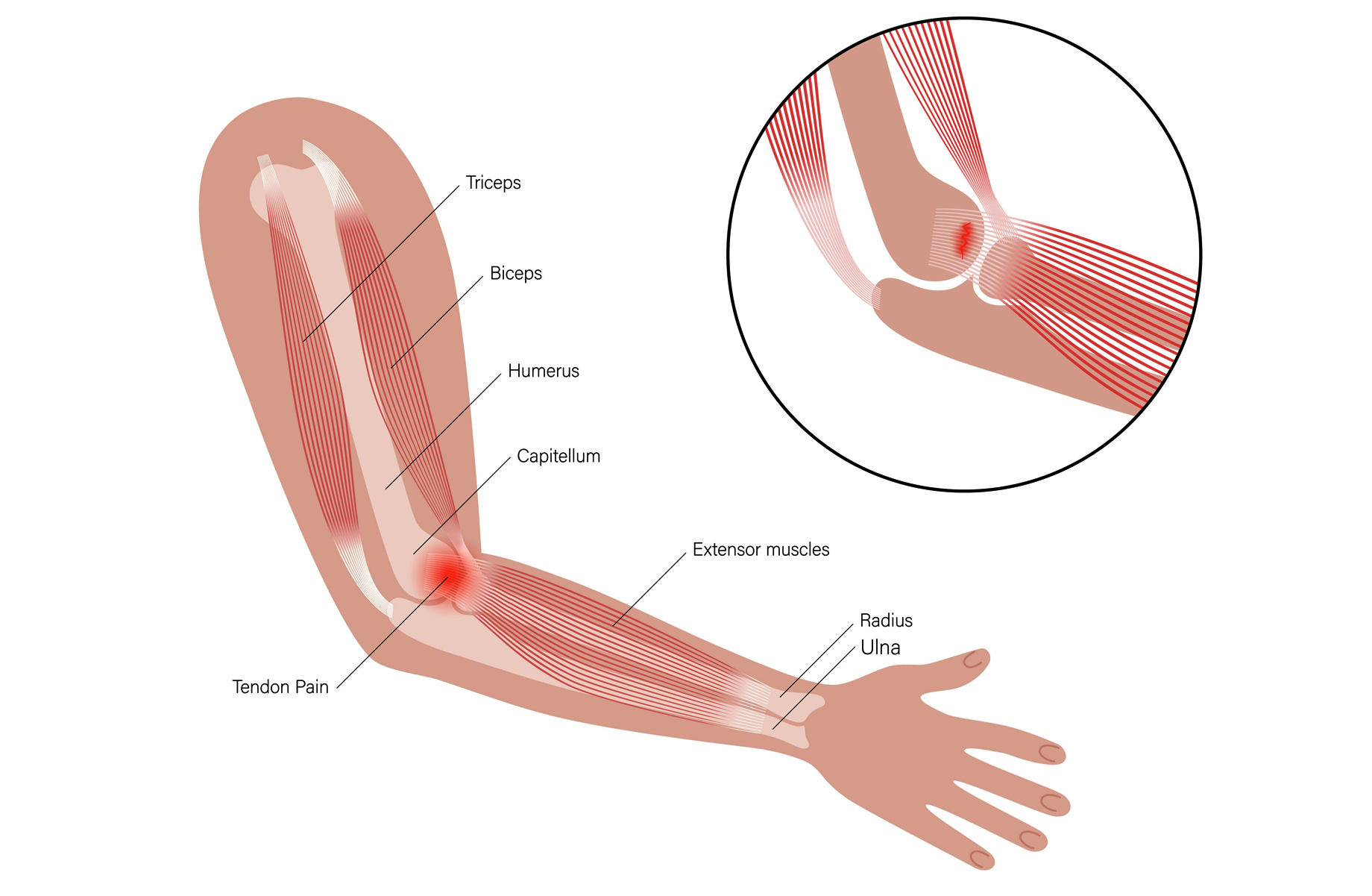
An illustration of a human arm displays key anatomical structures, including the triceps, biceps, humerus, capitellum, extensor muscles, radius, and ulna. Pain from lateral epicondylitis originates at the lateral aspect of the elbow and is commonly triggered by activities such as manipulating a doorknob, executing a backhand stroke in tennis, or lifting objects with the palm facing downward. Source: Veterans Affairs Canada (2024).
Medial epicondylitis (golfer's elbow)
Individuals with golfer's elbow predominantly report pain on the elbow's medial aspect (the side of the elbow that faces towards the body when the palm is oriented upwards), which may spread into the forearm (Figure 2: Medial epicondylitis). The pain intensifies during activities that involve wrist flexion (movement of the hand downwards towards the palm side) and pronation (rotational movement of the forearm that positions the palm downwards). Actions triggering this pain include swinging a golf club, performing a throwing motion, or grasping objects with the palm facing upwards. Medial epicondylitis is characterized by tenderness at the medial epicondyle and discomfort during tasks that demand wrist flexion against resistance and may lead to a decrease in grip strength.
Figure 2: Medial epicondylitis (golfer's elbow)
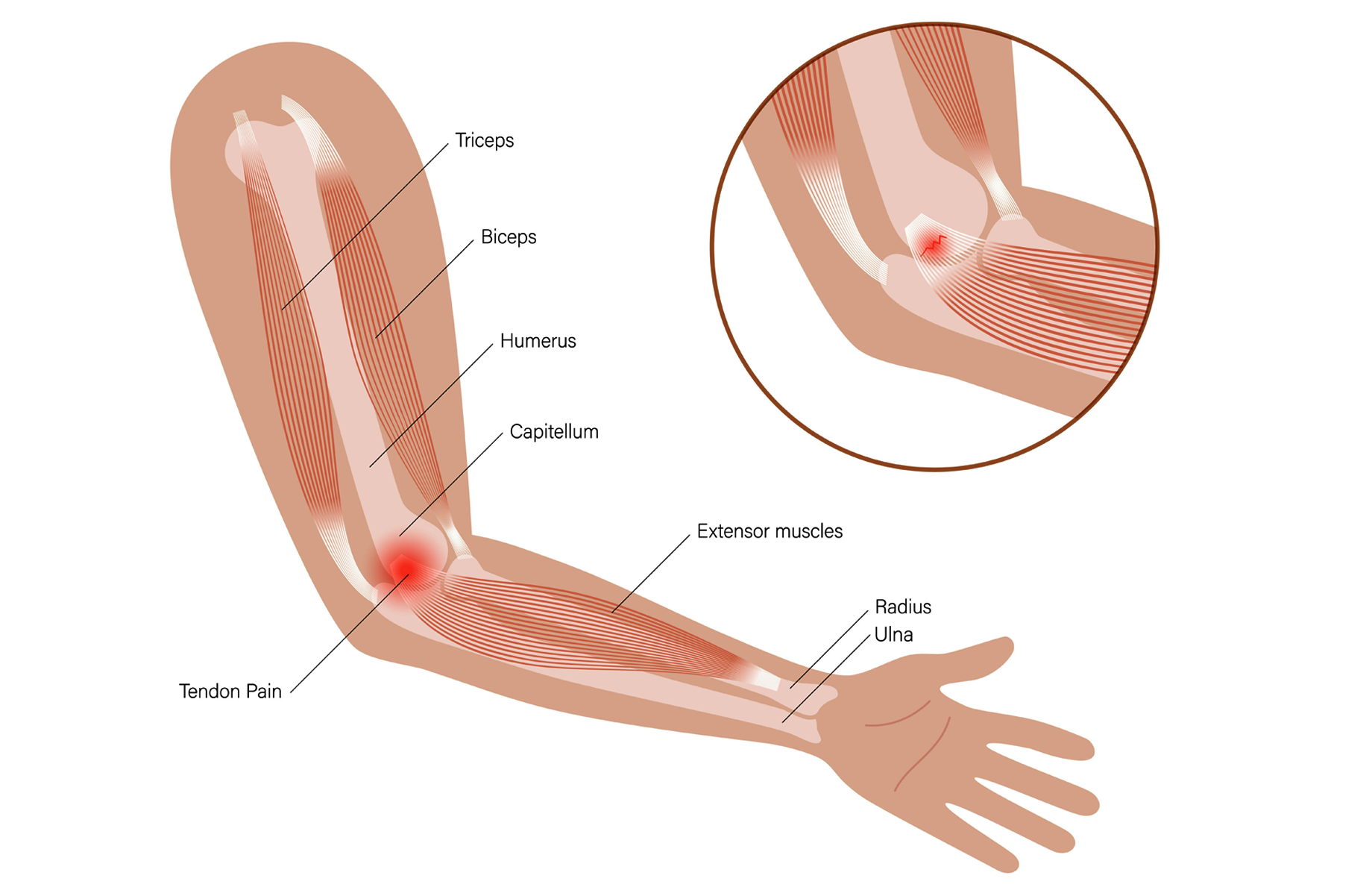
An illustration of a human arm displays key anatomical structures, including the triceps, biceps, humerus, capitellum, extensor muscles, radius, and ulna. Pain from medial epicondylitis originates at the medial aspect of the elbow and is commonly triggered by activities such as swinging, grasping, or throwing. Source: Veterans Affairs Canada (2024).
Both forms of epicondylitis, rooted in tendinopathy due to overuse or repetitive stress, distinctly compromise the ability to execute specific wrist and forearm movements associated with the extensor and flexor tendons.
Note: The duration of elbow tendinopathies usually ranges from weeks to months after which there is usually complete recovery.
Lateral elbow tendinopathies is typically seen in a middle-aged population (30-65 years) with an equal sex distribution. However, medial elbow tendinopathy typically affects people aged 40-60 years and more commonly affects female than male sex.
Entitlement considerations
In this section
Section A: Causes and/or aggravation
Section B: Medical conditions which are to be included in entitlement/assessment
Section A: Causes and/or aggravation
For VAC entitlement purposes, the following factors are accepted to cause or aggravate the conditions included in the Definition section of this EEG, and may be considered along with the evidence to assist in establishing a relationship to service. The factors have been determined based on a review of up-to-date scientific and medical literature, as well as evidence-based medical best practices. Factors other than those listed may be considered, however consultation with a disability consultant or medical advisor is recommended.
The timelines cited below are for guidance purposes. Each case should be adjudicated on the evidence provided and its own merits.
Factors
- Overuse:
- Performing forceful and repetitive activities with the hand or forearm on the affected side, or
- Performing forceful and sustained activities with the hand or forearm on the affected side.
Forceful means applying a substantial amount of force or pressure, using the muscles of the hand or forearm.
Repetitive means performing the same or similar hand or forearm movements repeatedly over time.
Sustained means for at least one hour per day, on more days than not, over at least three months before the clinical onset of chronic elbow tendinopathy. If specified activities have ceased before the clinical onset or aggravation of chronic elbow tendinopathy, then onset or aggravation must have occurred within 30 days of cessation.
Note: Activities with the hand or forearm that involve bending or straightening of the elbow; rotation, pronation, supination, twisting or screwing motion of the forearm; and flexion, extension or bending of the wrist or hand are examples of activities considered repetitive or forceful.
- Specific trauma to the soft tissue around the elbow joint prior to clinical onset or aggravation. For specific trauma to cause or aggravate chronic elbow tendinopathy, the following should be evident:
- within 24 hours of the injury, development of tenderness, pain, swelling, discoloration, or altered mobility, or any other pertinent sign or symptom, should occur in the elbow joint, and
- signs/symptoms should recur, either continuously or intermittently, from the time of the specific trauma to the time of diagnosis.
- Having one or more of the following systemic arthritic diseases at the time of clinical onset or aggravation of chronic elbow tendinopathy:
- ankylosing spondylitis
- Behcet syndrome
- gout or another crystal-induced arthropathy
- enteropathic spondyloarthropathy
- psoriatic arthropathy
- reactive arthritis
- rheumatoid arthritis
- undifferentiated spondyloarthropathy.
- Inability to obtain appropriate clinical management of chronic elbow tendinopathy.
Section B: Medical conditions which are to be included in entitlement/assessment
Section B provides a list of diagnosed medical conditions which are considered for VAC purposes to be included in the entitlement and assessment of chronic elbow tendinopathy. No included medical conditions were identified at the time of the publication of this EEG.
Section C: Common medical conditions which may result, in whole or in part, from chronic elbow tendinopathy and/or its treatment
No consequential medical conditions were identified at the time of the publication of this EEG. If the merits of the case and medical evidence indicate that a possible consequential relationship may exist, consultation with a disability consultant or medical advisor is recommended.
Links
Related VAC guidance and policy:
- Ankylosing Spondylitis – Entitlement Eligibility Guidelines
- Rheumatoid Arthritis – Entitlement Eligibility Guidelines
- Pain and Suffering Compensation – Policies
- Royal Canadian Mounted Police Disability Pension Claims – Policies
- Dual Entitlement – Disability Benefits – Policies
- Establishing the Existence of a Disability – Policies
- Disability Benefits in Respect of Peacetime Military Service – The Compensation Principle – Policies
- Disability Benefits in Respect of Wartime and Special Duty Service – The Insurance Principle – Policies
- Disability Resulting from a Non-Service Related Injury or Disease – Policies
- Consequential Disability – Policies
- Benefit of Doubt – Policies
References as of 22 January 2025
Australian Government Repatriation Medical Authority. (1997) Statement of Principles concerning epicondylitis (Balance of Probabilities) (53 of 1997). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. (1997) Statement of Principles concerning epicondylitis (Reasonable Hypothesis) (No.52 1997). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. Statement of Principles concerning epicondylitis (Balance of Probabilities) (No. 6 of 2023). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. Statement of Principles concerning epicondylitis (Reasonable Hypothesis) (No. 5 of 2023). SOPs - Repatriation Medical Authority
Beers, M. H., & Berkow, R. (1999). The Merck manual of diagnosis and therapy (17th ed.). Merck Research Laboratories.
Bretschneider, S. F., Los, F. S., Eygendaal, D., Kuijer, P. P. F. M., & van der Molen, H. F. (2022). Work‐relatedness of lateral epicondylitis: Systematic review including meta‐analysis and GRADE work‐relatedness of lateral epicondylitis. American Journal of Industrial Medicine, 65(1), 41–50. https://doi.org/10.1002/ajim.23303
Briggs, A. M., Cross, M. J., Hoy, D. G., Sànchez-Riera, L., Blyth, F. M., Woolf, A. D., & March, L. (2016). Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization World Report on Ageing and Health. The Gerontologist, 56(Suppl 2), S243–S255. https://doi.org/10.1093/geront/gnw002
Canosa-Carro, L., Bravo-Aguilar, M., Abuín-Porras, V., Almazán-Polo, J., García-Pérez-de-Sevilla, G., Rodríguez-Costa, I., López-López, D., Navarro-Flores, E., & Romero-Morales, C. (2022). Current understanding of the diagnosis and management of the tendinopathy: An update from the lab to the clinical practice. Disease-a-Month, 68(10), 101314. https://doi.org/10.1016/j.disamonth.2021.101314
Carpenter, D., & Draeger, R. W. (2021). Common Clinical Conditions of the Elbow. Clinical Foundations of Musculoskeletal Medicine: A Manual for Medical Students, 343-356.
Chumbley, E. M., O’Connor, F. G., & Nirschl, R. P. (2000). Evaluation of overuse elbow injuries. American Family Physician, 61(3), 691–700.
Curti, S., Mattioli, S., Bonfiglioli, R., Farioli, A., & Violante, F. S. (2021). Elbow tendinopathy and occupational biomechanical overload: A systematic review with best-evidence synthesis. Journal of Occupational Health, 63(1), e12186. https://doi.org/10.1002/1348-9585.12186
Dee, R. (Ed.). (1997). Principles of orthopaedic practice (2nd ed.). McGraw-Hill, Health Professions Division.
Descatha, A., Albo, F., Leclerc, A., Carton, M., Godeau, D., Roquelaure, Y., Petit, A., & Aublet‐Cuvelier, A. (2016). Lateral Epicondylitis and Physical Exposure at Work? A Review of Prospective Studies and Meta‐Analysis. Arthritis Care & Research, 68(11), 1681–1687. https://doi.org/10.1002/acr.22874
Descatha, A., Dale, A. M., Jaegers, L., Herquelot, E., & Evanoff, B. (2013). Self-reported physical exposure association with medial and lateral epicondylitis incidence in a large longitudinal study: Table 1. Occupational and Environmental Medicine, 70(9), 670–673. https://doi.org/10.1136/oemed-2012-101341
Descatha, A., Leclerc, A., Chastang, J. F., & Roquelaure, Y. (2003). Medial Epicondylitis in Occupational Settings: Prevalence, Incidence and Associated Risk Factors: Journal of Occupational and Environmental Medicine, 45(9), 993–1001. https://doi.org/10.1097/01.jom.0000085888.37273.d9
Dos Santos Bunn, P., De Oliveira Meireles, F., De Souza Sodré, R., Rodrigues, A. I., & Da Silva, E. B. (2021). Risk factors for musculoskeletal injuries in military personnel: A systematic review with meta-analysis. International Archives of Occupational and Environmental Health, 94(6), 1173–1189. https://doi.org/10.1007/s00420-021-01700-3
Fan, Z. J., Silverstein, B. A., Bao, S., Bonauto, D. K., Howard, N. L., Spielholz, P. O., Smith, C. K., Polissar, N. L., & Viikari‐Juntura, E. (2009). Quantitative exposure‐response relations between physical workload and prevalence of lateral epicondylitis in a working population. American Journal of Industrial Medicine, 52(6), 479–490. https://doi.org/10.1002/ajim.20700
Fauci, A. S., Braunwald, E., & Fuselbacher, K. J. (1998). Harrison's principles of internal medicine (14th ed). McGraw Hill.
Gold, J. E., d’Errico, A., Katz, J. N., Gore, R., & Punnett, L. (2009). Specific and non‐specific upper extremity musculoskeletal disorder syndromes in automobile manufacturing workers. American Journal of Industrial Medicine, 52(2), 124–132. https://doi.org/10.1002/ajim.20653
Golovach, I. Yu. (2021). Clinical significance of spondyloarthritis-attended enthesites: From pathophysiology to treatment (review). PAIN, JOINTS, SPINE, 11(1), 17–27. https://doi.org/10.22141/2224-1507.11.1.2021.226905
Haahr, J. P. (2003). Physical and psychosocial risk factors for lateral epicondylitis: A population based case-referent study. Occupational and Environmental Medicine, 60(5), 322–329. https://doi.org/10.1136/oem.60.5.322
Hadler, N. M. (1993). Occupational musculoskeletal disorders. Raven Press.
Herquelot, E., Bodin, J., Roquelaure, Y., Ha, C., Leclerc, A., Goldberg, M., Zins, M., & Descatha, A. (2013). Work‐related risk factors for lateral epicondylitis and other cause of elbow pain in the working population. American Journal of Industrial Medicine, 56(4), 400–409. https://doi.org/10.1002/ajim.22140
Ikeda, K., Yoshii, Y., Kohyama, S., Ikumi, A., Ikeda, R., & Yamazaki, M. (2023). Sex differences in wrist torque and endurance—Biomechanical factors associated with developing lateral epicondylitis of the humerus. Journal of Orthopaedic Research, 41(8), 1670–1677. https://doi.org/10.1002/jor.25506
Ikeda, K., Yoshii, Y., Kohyama, S., Ikumi, A., Ogawa, T., Ikeda, R., & Yamazaki, M. (2024). Pathophysiology of sex difference in refractoriness in lateral epicondylitis: Biomechanical study of wrist torque. Journal of Orthopaedic Research, 42(2), 277–285. https://doi.org/10.1002/jor.25684
Jayanthi, N. (2024). Patient Education: Elbow tendinopathy (tennis and golf elbow). UpToDate.
Keir, P. J., Farias Zuniga, A., Mulla, D. M., & Somasundram, K. G. (2021). Relationships and Mechanisms Between Occupational Risk Factors and Distal Upper Extremity Disorders. Human Factors: The Journal of the Human Factors and Ergonomics Society, 63(1), 5–31. https://doi.org/10.1177/0018720819860683
Kheiran, A., Pandey, A., & Pandey, R. (2021). Common tendinopathies around the elbow; what does current evidence say? Journal of Clinical Orthopaedics and Trauma, 19, 216–223. https://doi.org/10.1016/j.jcot.2021.05.021
Kim, M., Yoo, J.-I., Kim, M.-J., Na, J.-B., Lee, S.-I., & Park, K.-S. (2019). Prevalence of Upper Extremity Musculoskeletal Diseases and Disability among Fruit Tree Farmers in Korea: Cross-Sectional Study. Yonsei Medical Journal, 60(9), 870. https://doi.org/10.3349/ymj.2019.60.9.870
Koh, D., & Gan, W. H. (2022). Textbook of Occupational Medicine Practice (5th ed.). WORLD SCIENTIFIC. https://doi.org/10.1142/12512
Kraushaar, B. S., & Nirschl, R. P. (1999). Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. The Journal of Bone and Joint Surgery. American Volume, 81(2), 259–278.
Lovalekar, M., Hauret, K., Roy, T., Taylor, K., Blacker, S. D., Newman, P., Yanovich, R., Fleischmann, C., Nindl, B. C., Jones, B., & Canham-Chervak, M. (2021). Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. Journal of Science and Medicine in Sport, 24(10), 963–969. https://doi.org/10.1016/j.jsams.2021.03.016
Marinelli, A., Buondonno, C., Al Zoubi, A., & Guerra, E. (2023). Evaluation of Common Tendinopathies of the Elbow. In J. G. Lane, A. Gobbi, J. Espregueira-Mendes, C. C. Kaleka, & N. Adachi (Eds.), The Art of the Musculoskeletal Physical Exam (pp. 159–169). Springer International Publishing. https://doi.org/10.1007/978-3-031-24404-9_19
Mathew, A. J., Glintborg, B., Krogh, N. S., Hetland, M. L., & Østergaard, M. (2022). Enthesitis in patients with psoriatic arthritis and axial spondyloarthritis – data from the Danish nationwide DANBIO registry. Seminars in Arthritis and Rheumatism, 52, 151948. https://doi.org/10.1016/j.semarthrit.2021.12.012
Mease, P. J., Liu, M., Rebello, S., Hua, W., McLean, R. R., Yi, E., Park, Y., & Ogdie, A. (2020). Characterization of Patients With Axial Spondyloarthritis by Enthesitis Presence: Data from the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. ACR Open Rheumatology, 2(7), 449–456. https://doi.org/10.1002/acr2.11154
Millar, N. L., Silbernagel, K. G., Thorborg, K., Kirwan, P. D., Galatz, L. M., Abrams, G. D., Murrell, G. A. C., McInnes, I. B., & Rodeo, S. A. (2021). Tendinopathy. Nature Reviews Disease Primers, 7(1), 1. https://doi.org/10.1038/s41572-020-00234-1
Moore, K. L. (1985). Clinically oriented anatomy (2nd ed). Williams & Wilkins.
Niu, S. (2022). Diagnostic and Exposure Criteria for Occupational Diseases: Guidance Notes for Diagnosis and Prevention of the Diseases in the ILO List of Occupational Diseases (revised 2010) (C. Colosio, Ed.). International Labour Organisation.
Nordander, C., Ohlsson, K., Åkesson, I., Arvidsson, I., Balogh, I., Hansson, G.-Å., Strömberg, U., Rittner, R., & Skerfving, S. (2009). Risk of musculoskeletal disorders among females and males in repetitive/constrained work. Ergonomics, 52(10), 1226–1239. https://doi.org/10.1080/00140130903056071
O’Leary, T. J., Young, C. D., Wardle, S. L., & Greeves, J. P. (2023). Gender data gap in military research: A review of the participation of men and women in military musculoskeletal injury studies. BMJ Military Health, 169(1), 84–88. https://doi.org/10.1136/bmjmilitary-2021-002015
Park, H. B., Gwark, J.-Y., Im, J.-H., & Na, J.-B. (2021). Factors Associated With Lateral Epicondylitis of the Elbow. Orthopaedic Journal of Sports Medicine, 9(5), 232596712110077. https://doi.org/10.1177/23259671211007734
Piligian, G., Herbert, R., Hearns, M., Dropkin, J., Landsbergis, P., & Cherniack, M. (2000). Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity. American Journal of Industrial Medicine, 37(1), 75–93. https://doi.org/10.1002/(sici)1097-0274(200001)37:1<75::aid-ajim7>3.0.co;2-4
Purdam, C., & de Vos, R.-J. (2024). Tendinopathy. UpToDate.
Rhon, D. l I., Molloy, J. M., Monnier, A., Hando, B. R., & Newman, P. M. (2022). Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta-analysis. European Journal of Sport Science, 22(1), 16–34. https://doi.org/10.1080/17461391.2021.1931464
Rudzki, W., Delaney, T., & Macri, E. (2017). Military Personnel. In Brukner & Khan’s Clinical Sports Medicine: Injuries (5e ed., Vol. 1–1, pp. 991–1001). McGraw Hill. https://csm.mhmedical.com/content.aspx?bookid=1970§ionid=168697060
Salerno, S., & Giliberti, C. (2022). Women’s wrist and elbow at work: Analysis of acute injuries and cumulative trauma disorders to improve ergonomics in female-dominated activities. Ergonomics, 65(11), 1477–1485. https://doi.org/10.1080/00140139.2022.2095037
Sammito, S., Hadzic, V., Karakolis, T., Kelly, K. R., Proctor, S. P., Stepens, A., White, G., & Zimmermann, W. O. (2021). Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Military Medical Research, 8(1), 66. https://doi.org/10.1186/s40779-021-00357-w
Scott, A., Purdam, C. R., & Physio, D. M. S. (2023). Overview of the management of overuse (persistent) tendinopathy. UpToDate.
Seidel, D. H., Ditchen, D. M., Hoehne-Hückstädt, U. M., Rieger, M. A., & Steinhilber, B. (2019). Quantitative Measures of Physical Risk Factors Associated with Work-Related Musculoskeletal Disorders of the Elbow: A Systematic Review. International Journal of Environmental Research and Public Health, 16(1), 130. https://doi.org/10.3390/ijerph16010130
Sérazin, C., Ha, C., Bodin, J., Imbernon, E., & Roquelaure, Y. (2013). Employment and occupational outcomes of workers with musculoskeletal pain in a French region. Occupational and Environmental Medicine, 70(3), 143–148. https://doi.org/10.1136/oemed-2012-100685
Shiri, R., & Viikari-Juntura, E. (2011). Lateral and medial epicondylitis: Role of occupational factors. Best Practice & Research Clinical Rheumatology, 25(1), 43–57. https://doi.org/10.1016/j.berh.2011.01.013
Shiri, R., Viikari-Juntura, E., Varonen, H., & Heliovaara, M. (2006). Prevalence and Determinants of Lateral and Medial Epicondylitis: A Population Study. American Journal of Epidemiology, 164(11), 1065–1074. https://doi.org/10.1093/aje/kwj325
Siegel, I. M. (1990). Orthopedic Pathophysiology In Diagnosis and Treatment. JAMA: The Journal of the American Medical Association, 264(19), 2576. https://doi.org/10.1001/jama.1990.03450190108039
Sluiter, J. K., Rest, K. M., & Frings-Dresen, M. H. (2001). Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scandinavian Journal of Work, Environment & Health, 27 Suppl 1, 1–102.
Stolwijk, C., van Tubergen, A., Castillo-Ortiz, J. D., & Boonen, A. (2015). Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: A systematic review and meta-analysis. Annals of the Rheumatic Diseases, 74(1), 65–73. https://doi.org/10.1136/annrheumdis-2013-203582
Sunar, I., Ataman, S., Nas, K., Kilic, E., Sargin, B., Kasman, S. A., Alkan, H., Sahin, N., Cengiz, G., Cuzdan, N., Gezer, I. A., Keskin, D., Mülkoğlu, C., Resorlu, H., Bal, A., Duruöz, M. T., Küçükakkaş, O., Yurdakul, O. V., Melikoglu, M. A., … Tuncer, T. (2020). Enthesitis and its relationship with disease activity, functional status, and quality of life in psoriatic arthritis: A multi-center study. Rheumatology International, 40(2), 283–294. https://doi.org/10.1007/s00296-019-04480-9
Tsechelidis, O. B., Sabido-Sauri, R., & Aydin, S. Z. (2023). Enthesitis in Spondyloarthritis Including Psoriatic Arthritis—To Inject or Not To Inject?: A Narrative Review. Clinical Therapeutics, 45(9), 852–859. https://doi.org/10.1016/j.clinthera.2023.08.002
Tubergen, A. (2024). Overview of the clinical manifestations and classification of spondyloarthritis. UpToDate.
van Rijn, R. M., Huisstede, B. M. A., Koes, B. W., & Burdorf, A. (2008). Associations between work-related factors and specific disorders at the elbow: A systematic literature review. Rheumatology, 48(5), 528–536. https://doi.org/10.1093/rheumatology/kep013
Veterans Affairs Canada (2024). Lateral Epicondylitis. License for use purchased from https://www.123rf.com/photo_168794398_pain-in-human-arm-lateral-epicondylitis-tennis-elbow-trauma-or-inflammation-in-hand-muscular.html
Veterans Affairs Canada (2024). Medial Epicondylitis. License for use purchased from https://www.123rf.com/photo_168794406_medial-epicondylitis-golfer-elbow.html
Walker-Bone, K., Palmer, K. T., Reading, I., Coggon, D., & Cooper, C. (2012). Occupation and epicondylitis: A population-based study. Rheumatology, 51(2), 305–310. https://doi.org/10.1093/rheumatology/ker228
Weinstein, S. L., Buckwalter, J. A., & Turek, S. L. (Eds.). (1994). Turek’s Orthopaedics: Principles and their application (5th ed). Lippincott.
Wijnhoven, H. A. H., De Vet, H. C. W., & Picavet, H. S. J. (2006). Prevalence of musculoskeletal disorders is systematically higher in women than in men. The Clinical Journal of Pain, 22(8), 717–724. https://doi.org/10.1097/01.ajp.0000210912.95664.53
Wolf, J. M. (2023). Lateral Epicondylitis. New England Journal of Medicine, 388(25), 2371–2377. https://doi.org/10.1056/NEJMcp2216734
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/