Entitlement Eligibility Guideline (EEG)
Date reviewed: 31 March 2025
Date created: February 2005
ICD-11 codes: FA00-03, FA0Z
VAC medical codes:
71830
Acromioclavicular separation/osteoarthritis
71510
Osteoarthritis shoulder joint
71520
Osteoarthritis elbow
71530
Osteoarthritis wrist
71540
Osteoarthritis of all finger joints and joints of thumbs
01346
Osteoarthritis hip
01341
Tibiofemoral osteoarthritis, osteoarthritis knee, patellofemoral osteoarthritis
01348
Osteoarthritis ankle
71537
Osteoarthritis of foot joints
This publication is available upon request in alternate formats.
Full document – PDF Version
Definition
Osteoarthritis (OA) is a common joint condition that occurs when the protective cushioning between the bones, called cartilage, starts to wear away. This can result in bones rubbing against each other, leading to pain, swelling, and stiffness in the affected joint.
Note: The terms osteoarthritis and osteoarthrosis are used interchangeably in the medical community. For this guideline's purposes, these terms are considered synonymous and will be hereinafter called OA.
Inclusions:
For the purposes of this entitlement eligibility guideline (EEG), the following conditions are included and are considered equivalent. They will hereinafter be referred to as OA:
- osteoarthritis
- osteoarthrosis
- degenerative arthritis
- degenerative joint disease
- non-inflammatory arthritis.
Exclusions:
This EEG excludes OA of the following joints. Please refer to their respective EEG:
This EEG excludes inflammatory joint diseases, including, but not limited to:
- rheumatoid arthritis
- Reiter's syndrome
- psoriatic arthritis
- ankylosing spondylitis (peripheral joints)
- septic arthritis
- arthritis associated with Crohn’s disease
- arthritis associated with ulcerative colitis.
This EEG excludes depositional joint diseases, including but not limited to:
- gout and pseudogout
- hemochromatosis
- Wilson’s disease
- ochronosis (alkaptonuria)
- hemophilia and other bleeding disorders.
Diagnostic standard
A diagnosis from a qualified physician, nurse practitioner, or physician assistant (within their scope of practice) is required.
- OA is typically diagnosed through a combination of a medical history, physical examination, and diagnostic tests.
- For Veterans Affairs Canada (VAC) entitlement purposes, a disability resulting from OA must be present, demonstrated by the presence of relevant signs and/or symptoms of OA on clinical exam.
- Diagnostic imaging as evidence of OA is insufficient alone to establish a diagnosis as the condition must be symptomatic. Imaging findings do not always correlate with symptoms of OA.
- Each claimed joint should be individually diagnosed with OA and should describe the site(s) affected.
- The term OA of the hand and OA of the foot may be used where five or more joints in these areas are affected by OA. For VAC entitlement purposes, each hand is considered one joint, and each foot is considered one joint.
Note: For VAC purposes, the diagnosis of “generalized OA” is not accepted. Each joint must be entitled individually, except for multiple joints in the hand and foot.
Anatomy and physiology
A joint is a connection point where two or more bones come together. To make sure the bones can move smoothly without rubbing against each other, there are a few important parts:
- Bones provide structural support, internal organ protection, and attachment points for muscles and tendons to allow movement.
- Cartilage acts as a cushion, covering the end of the bone at the joint. Cartilage ensures bones glide smoothly and prevents rubbing during movement.
- Synovium provides a thin layer that lines the inside of the joint. Synovium makes synovial fluid which lubricates the joint and reduces friction.
- Ligaments are made of strong bands of tissue that connect the bones together at the joint. Ligaments help to give the joint stability and prevent excessive movement.
- Muscles surround the joint and help to control the coordination of movement by the joint.
- The joint capsule is a strong, flexible covering around the joint which holds components in place and provides stability to the joint.
There are several different types of joints within the human body with each type serving different purposes and allowing various types of movement. The main types of joints, with examples, are outlined below:
- Hinge joints allow movement in only one direction, such as bending and straightening. Examples include the knee and elbow joints.
- Ball-and-socket joints: allow a wide range of movement in many directions, including rotation. The rounded end of one bone fits into a cup-like socket of another bone. Examples include the hip and shoulder joints.
- Pivot joints allow bones to rotate around each other. Examples include joints in the neck and in the forearm.
- Condyloid joints allow movement in two directions, such as bending and straightening, and as well, side to side motion. An example is the joint at the base of the fingers.
- Saddle joints are similar to condyloid joints but allow a greater range of movement. An example is the thumb joint.
- Gliding (plane) joints allow bones to slide past each other in various directions. Examples include the wrists and ankles.
- Fixed (fibrous) joints are immovable and are held together by tough connective tissue. Examples include the sutures in the skull.
- Cartilaginous joints have a layer of cartilage between the bones, allowing limited movement. An example is between the vertebrae in the spine.
OA is a common type of arthritis.
OA starts when the protective cartilage providing joint cushioning begins to wear away. When the cartilage wears away, the bones may start to rub against each other, which can cause irritation and small injuries to the bones. The body tries to repair these injuries but cannot keep up with repairs. As time progresses, the joint can become inflamed causing pain, swelling, and stiffness. Many factors can contribute to the development of OA including genetics, joint injuries, and lifestyle.
For example, Figure 1: Knee joint osteoarthritis depicts a normal knee joint as compared to a knee joint with OA.
Figure 1: Knee joint osteoarthritis
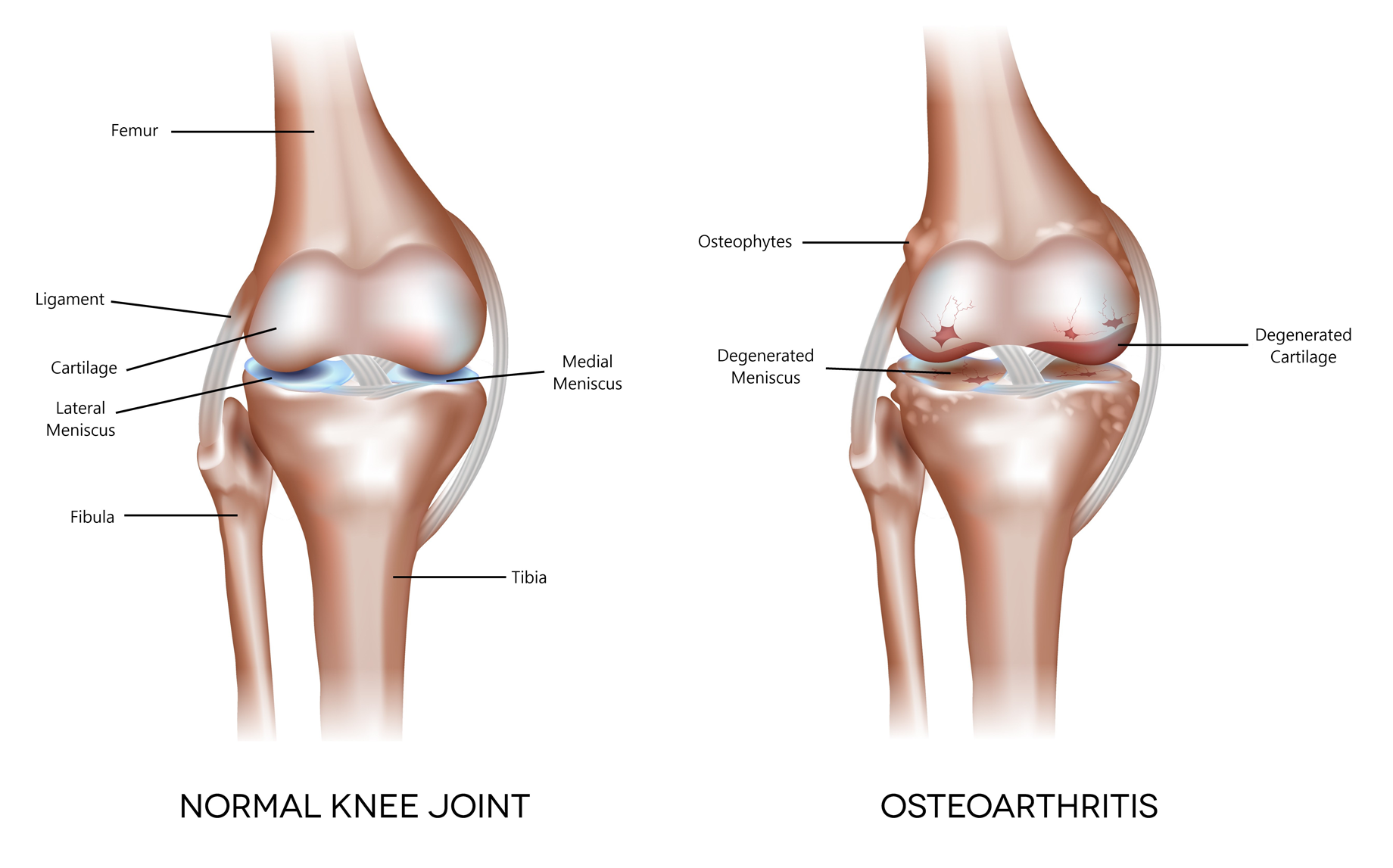
A close-up of a normal, healthy knee joint (left) reveals the internal structures including the femur, ligaments, cartilage, fibula, and tibia. The healthy joint features smooth cartilage and well-defined lateral and medial menisci, allowing for stable, pain-free movement. In contrast, a knee joint with osteoarthritis (right) shows degenerated cartilage and menisci, along with the presence of osteophytes (bone spurs), leading to inflammation and reduced mobility. Source: Veterans Affairs Canada (2024).
As the cartilage continues to thin out, the body may form new bone growth called osteophytes. The inflammation, ongoing repair attempts, and changes in the joint’s structure, can lead to symptoms of OA. This usually happens gradually and can affect the joint’s function.
After the initial stages of cartilage degeneration, there may be a delay of many years before a person feels joint pain or x-ray evidence of osteoarthritic changes develop. Significant cartilage damage may have occurred before relevant signs and symptoms appear.
For example, Figure 2: Hip joint osteoarthritis depicts of a normal hip joint as compared to a hip joint with OA.
Figure 2: Hip joint osteoarthritis
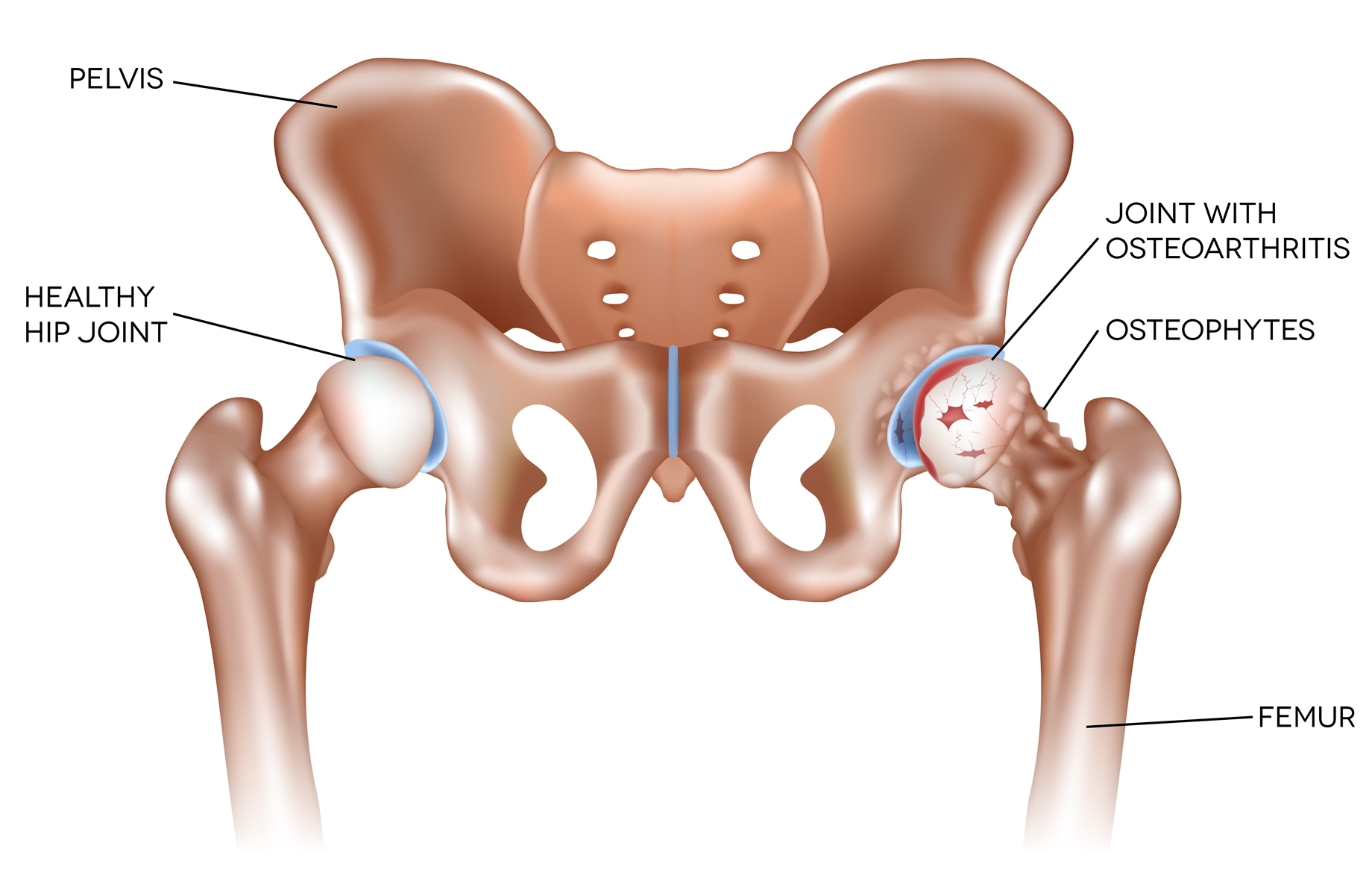
A healthy hip joint (left) features smooth cartilage that enables pain-free, fluid movement. In contrast, a hip joint with osteoarthritis (right) shows worn cartilage, the presence of osteophytes (bone spurs), and results in stiffness and pain. Source: Veterans Affairs Canada (2024).
OA is a common disease, with more than 75% of individuals over 70 years of age showing evidence of OA. While the incidence of OA increases with age, the disease is not caused solely by joint aging. Joint trauma and other factors can cause or accelerate the development of OA.
Clinical features
The primary symptoms of OA are joint pain, stiffness, and restricted movement. Pain associated with OA is usually worse with joint use and relieved with rest; however, it may persist when the advanced stages of the disease are reached. The pain can range from a sharp discomfort to a constant ache. Pain is typically subtle at onset, and gradually progresses, usually for many years. Flare-ups of discomfort may be followed by partial or complete remission. Joints often feel stiff after periods of rest, with improvement in the stiffness as the joint resumes moving.
OA is most often observed in the knees, hips, fingers, hands and back. The elbow, wrist, shoulder, and ankle are less commonly affected.
Structural joint changes may be present in the absence of symptoms and vice versa. There are known inconsistencies between findings on x-rays and clinical symptoms, with only 50 to 60% of people with radiographic changes having symptoms of OA. Clinical symptoms, which must be recurrent or continuous after initial manifestation, can precede x-ray findings by up to 10 years.
Examination of the involved joints may reveal mild tenderness, pain, restricted range of movement, joint effusions, and crepitus. In advanced OA, obvious deformity, bony enlargement, angulation, and marked loss of joint movement can be seen.
Female biological sex is associated with a higher prevalence and severity of OA. OA of the hands and knees is more common in females, whereas OA of the hips is more common in males. The reason for the increased risk of OA in females is unclear, but may be related to hormones, genetics, or other undetermined factors.
Military service members experience incidence rates for acute traumatic joint injuries significantly higher than rates observed in the general population. Acute traumatic joint injury has been identified as an important risk factor for OA.
Entitlement considerations
In this section
Section A: Causes and/or aggravation
Section B: Medical conditions which are to be included in entitlement/assessment
Section A: Causes and/or aggravation
For VAC entitlement purposes, the following factors are accepted to cause or aggravate the conditions included in the Definition section of this EEG, and may be considered along with the evidence to assist in establishing a relationship to service. The factors have been determined based on a review of up-to-date scientific and medical literature, as well as evidence-based medical best practices. Factors other than those listed may be considered, however consultation with a disability consultant or medical advisor is recommended.
The timelines cited below are for guidance purposes. Each case should be adjudicated on the evidence provided and its own merits.
Factors
- Having experienced a trauma to the affected joint prior to clinical onset or aggravation of OA. Trauma to the affected joint means a discrete event involving the application of significant physical force to, or through, the affected joint that causes damage to the joint with clinical symptoms developing within 24 hours of the event and persisting for at least seven days.
- Having experienced forceful or repetitive activities using the affected joint of the upper limb listed below prior to clinical onset or aggravation of OA:
- glenohumeral
- acromioclavicular
- elbow
- wrist
- hand.
For forceful or repetitive activity to cause and/or aggravate OA in one of the above joints, the following criteria should be met:
- for an average of at least 100 hours per month; and
- a cumulative period of at least 10 years within a 15 year period; and
- signs/symptoms of OA should occur within 25 years of the activity ceasing.
Forceful or repetitive activity using the upper limb is defined as repeated or sustained pinch grip or hand/power grip.
- Having experienced significant vibration to the affected joint of the upper limb as listed below prior to the clinical onset or aggravation of OA:
- elbow
- wrist
- hand.
For vibration to cause and/or aggravate OA in the elbow, wrist or hand, the following criteria should be met:
- the use of a hand-held, vibrating, percussion tool or object on more days than not; and
- over a cumulative period of at least ten years; and
- signs/symptoms of OA should occur during the activity producing the vibration, or within 25 years of the activity ceasing.
Vibration can occur from a number of tools, including pneumatic tools and other mechanized tools, such as a chain saw.
A pneumatic tool is any tool driven by compressed air, including but not limited to jack hammers, pneumatic drills, compacters, large pop rivet guns of the type used on construction sites, sand blasting equipment, and spray-painting equipment.
- Having class 3/severe obesity (defined as body mass index [BMI] of 40 or greater) for at least ten years before the clinical onset or aggravation of OA in following joints:
- hip
- knee.
- Having an amputation involving either leg before the clinical onset or aggravation of OA in the following joints:
- hip
- knee.
- Having a permanent and uncorrected leg length inequality (LLI), as outlined in the LLI discussion paper, before the clinical onset or aggravation of OA in the following joints:
- hip
- knee.
- Having a service period lasting 10 full time equivalent (FTE) years or more involving rigorous service activities, tactical training, and maintenance of physical fitness, where the clinical onset or aggravation of OA of the following joints has occurred within 25 years of release from service:
- hip
- knee
- ankle.
Note: VAC accepts the development of OA of the above joints having a service period of at least five FTE years for:
- an anatomically abnormal hip, knee, or ankle; or
- female biological sex; or
- evidence of hip, knee, or ankle symptoms documented during service.
- Prolonged kneeling or squatting using the affected joints of the lower limbs as listed below, prior to the clinical onset or aggravation of OA:
- hip
- knee.
For prolonged kneeling or squatting to contribute to the development of OA in the above joints, the following criteria should be met:
- a cumulative period of at least one hour per day, on more days than not, for a continuous period of at least three years before the clinical onset or aggravation of OA in that joint; and
- where the clinical onset or aggravation of OA in that joint occurs within the 25 years following that period.
- Having Paget’s disease of the bone of the affected joint before the clinical onset or aggravation of OA in that joint.
- Having acromegaly before the clinical onset or aggravation of OA in that joint.
- Having femoroacetabular impingement syndrome of the affected joint, before the clinical onset or aggravation of OA in that joint, for OA of the hip joint only.
- Having joint instability or dislocation of the affected joint, at least one year before the clinical onset or aggravation of OA in that joint.
- Having neuropathic arthropathy prior to clinical onset or aggravation of OA. Neuropathic arthropathy is a neurologic disorder that causes a loss of sensory nerve functions which is accompanied by destructive arthropathy similar to OA. The lack of normal joint sensation alone is not sufficient to result in neuropathic arthropathy.
- Having necrosis of the subchondral bone near the affected joint, before the clinical onset or aggravation of OA in that joint.
- Having disordered joint mechanics (malalignment) of the affected joint for at least five years before the clinical onset or aggravation of OA in that joint.
Disordered joint mechanics is defined as structural maldistribution of loading forces on that joint resulting from:
- a rotation or angulation deformity of the bones of the affected limb; or
- a rotation or angulation deformity of the joints of the affected limb; or
- a rotation or angulation deformity of the bones adjacent to the affected joint.
- Inability to obtain appropriate clinical management for OA.
Section B: Medical conditions which are to be included in entitlement/assessment
Section B provides a list of diagnosed medical conditions which are considered for VAC purposes to be included in the entitlement and assessment of OA of the affected joint.
OA includes all entitled soft tissue and joint disorders in the area of the affected joint. Examples include, but are not limited to the following:
- OA of the glenohumeral joint of the shoulder
- Adhesive capsulitis
- Rotator cuff syndrome/rotator cuff disease
- Subacromial impingement syndrome
- Calcific tendinitis
- Supraspinatus tendonitis
- Subacromial bursitis
- Labral tear shoulder
- SLAP lesion shoulder
- Rotator cuff tendonitis
- OA of the cervical spine
- OA of the thoracic spine
- Degenerative disc disease of thoracic spine
- Thoracic disc disease
- Thoracic spondylosis
- Facet joint syndrome thoracic spine
- Chronic mechanical thoracic pain
- Chronic thoracic sprain/strain
- Chronic myofascial pain of the thoracic spine region
- OA of the lumbar spine
- OA of the hip
- Chronic trochanteric bursitis
- Labral tear of the hip
- OA of the knee
- Chondromalacia patellae
- Patellofemoral syndrome
- Internal derangement of the knee
- Patellofemoral OA
- Prepatellar bursitis
- Suprapatellar bursitis
- Medial and lateral collateral ligamentous sprain
- Meniscus tear
- Baker’s cyst
- Chronic plica syndrome
- Anterior cruciate ligament tear
- Posterior cruciate ligament tear
- OA of the ankle
- Chronic ankle sprain
- Calcaneal bursitis
- Achilles tendonitis
- OA of the wrist
- OA of all fingers and thumbs
- OA of the elbow
- Chronic olecranon bursitis
- Chronic medial epicondylitis
- Chronic lateral epicondylitis
- Exostosis of olecranon
- OA of the temporomandibular joint
Section C: Common medical conditions which may result, in whole or in part, from osteoarthritis and/or its treatment
No consequential medical conditions were identified at the time of the publication of this EEG. If the merits of the case and medical evidence indicate that a possible consequential relationship may exist, consultation with a disability consultant or medical advisor is recommended.
Links
Related VAC guidance and policy:
- Ankylosing Spondylitis – Entitlement Eligibility Guidelines
- Chronic Achilles Tendon Conditions - Entitlement Eligibility Guidelines
- Chronic Elbow Tendinopathy (Epicondylitis) – Entitlement Eligibility Guidelines
- Chronic Plica Syndrome – Entitlement Eligibility Guidelines
- Cervical Spine Conditions – Entitlement Eligibility Guidelines
- Internal Derangement Knee – Entitlement Eligibility Guidelines
- Leg Length Inequality (LLI) – Discussion Paper
- Lumbar Spine Conditions - Entitlement Eligibility Guidelines
- Paget's Disease of Bone (Osteitis Deformans) - Entitlement Eligibility Guidelines
- Rheumatoid Arthritis – Entitlement Eligibility Guidelines
- Rotator Cuff Disease – Entitlement Eligibility Guidelines
- Temporomandibular Disorders – Entitlement Eligibility Guidelines
- Pain and Suffering Compensation - Policies
- Royal Canadian Mounted Police Disability Pension Claims - Policies
- Dual Entitlement – Disability Benefits - Policies
- Establishing the Existence of a Disability - Policies
- Disability Benefits in Respect of Peacetime Military Service – The Compensation Principle - Policies
- Disability Benefits in Respect of Wartime and Special Duty Service – The Insurance Principle - Policies
- Disability Resulting from a Non-Service Related Injury or Disease - Policies
- Consequential Disability - Policies
- Benefit of Doubt - Policies
References as of 31 March 2025
Altman, R., Asch, E., Bloch, D., Bole, G., Borenstein, D., Brandt, K., Christy, W., Cooke, T. D., Greenwald, R., Hochberg, M., Howell, D., Kaplan, D., Koopman, W., Longley, S., Mankin, H., McShane, D. J., Medsger, T., Meenan, R., Mikkelsen, W., Wolfe, F. (1986). Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis & Rheumatism, 29(8), 1039–1049. https://doi.org/10.1002/art.1780290816
Anderson, J. J., & Felson, D. T. (1988). Factors associated with osteoarthritis of the knee in the first national health and nutrition examination survey (Hanes I). American Journal of Epidemiology, 128(1), 179–189. https://doi.org/10.1093/oxfordjournals.aje.a114939
Australian Government Repatriation Medical Authority. (2001). Statement of Principles concerning osteoarthritis (Balance of probabilities) (No. 82 of 2001). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. (2001). Statement of Principles concerning osteoarthritis (Reasonable Hypothesis) (No. 81 of 2001). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. (2022). Statement of Principles concerning osteoarthritis (Balance of probabilities) (No. 62 of 2017). SOPs - Repatriation Medical Authority
Australian Government Repatriation Medical Authority. (2022). Statement of Principles concerning osteoarthritis (Reasonable Hypothesis) (No. 61 of 2017). SOPs - Repatriation Medical Authority
Badley, E. M., Wilfong, J. M., Yip, C., Millstone, D. B., & Perruccio, A. V. (2020). The contribution of age and obesity to the number of painful joint sites in individuals reporting osteoarthritis: A population-based study. Rheumatology, 59(11), 3350–3357. https://doi.org/10.1093/rheumatology/keaa138
Barbe, M. F., Massicotte, V. S., Assari, S., Monroy, M. A., Frara, N., Harris, M. Y., Amin, M., King, T., Cruz, G. E., & Popoff, S. N. (2018). Prolonged high force high repetition pulling induces osteocyte apoptosis and trabecular bone loss in distal radius, while low force high repetition pulling induces bone anabolism. Bone, 110, 267–283. https://doi.org/10.1016/j.bone.2018.02.014
Batushansky, A., Zhu, S., Komaravolu, R. K., South, S., Mehta-D’Souza, P., & Griffin, T. M. (2022). Fundamentals of OA. An initiative of Osteoarthritis and Cartilage. Obesity and metabolic factors in OA. Osteoarthritis and Cartilage, 30(4), 501–515. https://doi.org/10.1016/j.joca.2021.06.013
Beebe, G. W. (1975). Follow-up studies of World War II and Korean war prisoners. American Journal of Epidemiology, 101(5), 400–422. https://doi.org/10.1093/oxfordjournals.aje.a112108
Bergmann, A., Bolm-Audorff, U., Krone, D., Seidler, A., Liebers, F., Haerting, J., Freiberg, A., & Unverzagt, S. (2017). Occupational Strain as a Risk for Hip Osteoarthritis. Deutsches Ärzteblatt International. https://doi.org/10.3238/arztebl.2017.0581
Berkow, R., Fletcher, A. J., & Bondy, P. K. (1992). The Merck Manual of Diagnosis and Therapy. Merck Research Laboratories. https://books.google.ca/books?id=GdU-0AEACAAJ
Briggs, A. M., Cross, M. J., Hoy, D. G., Sànchez-Riera, L., Blyth, F. M., Woolf, A. D., & March, L. (2016). Musculoskeletal Health Conditions Represent a Global Threat to Healthy Aging: A Report for the 2015 World Health Organization World Report on Ageing and Health. The Gerontologist, 56(Suppl 2), S243–S255. https://doi.org/10.1093/geront/gnw002
Burant, C. J., Graham, G. C., Deimling, G., Kresevic, D., Kahana, E., Wykle, M., Kwoh, C. K., & Ibrahim, S. A. (2023). The effects of osteoarthritis on depressive symptomatology among older U.S. military Veterans. The International Journal of Aging & Human Development, 96(3), 267–284. https://doi.org/10.1177/00914150221084952
Burry, H. C. (1987). Sport, exercise, and arthritis. Rheumatology, 26(5), 386–388. https://doi.org/10.1093/rheumatology/26.5.386
Canetti, E. F. D., Schram, B., Orr, R. M., Knapik, J., & Pope, R. (2020). Risk factors for development of lower limb osteoarthritis in physically demanding occupations: A systematic review and meta-analysis. Applied Ergonomics, 86, 103097. https://doi.org/10.1016/j.apergo.2020.103097
Chen, L., Zheng, J. J. Y., Li, G., Yuan, J., Ebert, J. R., Li, H., Papadimitriou, J., Wang, Q., Wood, D., Jones, C. W., & Zheng, M. (2020). Pathogenesis and clinical management of obesity-related knee osteoarthritis: Impact of mechanical loading. Journal of Orthopaedic Translation, 24, 66–75. https://doi.org/10.1016/j.jot.2020.05.001
Coggon, D., Croft, P., Kellingray, S., Barrett, D., McLaren, M., & Cooper, C. (2000). Occupational physical activities and osteoarthritis of the knee. Arthritis & Rheumatism, 43(7), 1443–1449. https://doi.org/10.1002/1529-0131(200007)43:7<1443::AID-ANR5>3.0.CO;2-1
Cooper, C., McAlindon, T., Coggon, D., Egger, P., & Dieppe, P. (1994). Occupational activity and osteoarthritis of the knee. Annals of the Rheumatic Diseases, 53(2), 90–93. https://doi.org/10.1136/ard.53.2.90
Coppack, R. J., Bilzon, J. L., Wills, A. K., Papadopoulou, T., Cassidy, R. P., Nicol, A. M., & Bennett, A. N. (2022). The test–retest reliability of the Military Physical Loading Questionnaire (MPLQ). BMJ Military Health, 168(4), 273–278. https://doi.org/10.1136/bmjmilitary-2020-001404
d’Errico, A., Fontana, D., Sebastiani, G., & Ardito, C. (2023). Risk of symptomatic osteoarthritis associated with exposure to ergonomic factors at work in a nationwide Italian survey. International Archives of Occupational and Environmental Health, 96(1), 143–154. https://doi.org/10.1007/s00420-022-01912-1
dos Santos Bunn, P., de Oliveira Meireles, F., de Souza Sodré, R., Rodrigues, A. I., & da Silva, E. B. (2021). Risk factors for musculoskeletal injuries in military personnel: A systematic review with meta-analysis. International Archives of Occupational and Environmental Health, 94(6), 1173–1189. https://doi.org/10.1007/s00420-021-01700-3
Ding, H., Solovieva, S., Vehmas, T., Takala, E.-P., & Leino-Arjas, P. (2010). Hand osteoarthritis and pinch grip strength among middle-aged female dentists and teachers. Scandinavian Journal of Rheumatology, 39(1), 84–87. https://doi.org/10.3109/03009740903201834
Duclos, M. (2016). Osteoarthritis, obesity and type 2 diabetes: The weight of waist circumference. Annals of Physical and Rehabilitation Medicine, 59(3), 157–160. https://doi.org/10.1016/j.rehab.2016.04.002
Ernst, E. (1993). Smoking, a cause of back trouble? Rheumatology, 32(3), 239–242. https://doi.org/10.1093/rheumatology/32.3.239
Farrokhi, S., Mazzone, B., Yoder, A., Grant, K., & Wyatt, M. (2016). A Narrative Review of the Prevalence and Risk Factors Associated With Development of Knee Osteoarthritis After Traumatic Unilateral Lower Limb Amputation. Military Medicine, 181(S4), 38–44. https://doi.org/10.7205/MILMED-D-15-00510
Felson, D. T., Hannan, M. T., Naimark, A., Berkeley, J., Gordon, G., Wilson, P. W., & Anderson, J. (1991). Occupational physical demands, knee bending, and knee osteoarthritis: Results from the Framingham Study. The Journal of Rheumatology, 18(10), 1587–1592.
Felson, D. T., Lawrence, R. C., Dieppe, P. A., Hirsch, R., Helmick, C. G., Jordan, J. M., Kington, R. S., Lane, N. E., Nevitt, M. C., Zhang, Y., Sowers, M., McAlindon, T., Spector, T. D., Poole, A. R., Yanovski, S. Z., Ateshian, G., Sharma, L., Buckwalter, J. A., Brandt, K. D., & Fries, J. F. (2000). Osteoarthritis: New insights. Part 1: the disease and its risk factors. Annals of Internal Medicine, 133(8), 635–646. https://doi.org/10.7326/0003-4819-133-8-200010170-00016
Felson, D. T., Zhang, Y., Hannan, M. T., Naimark, A., Weissman, B. N., Aliabadi, P., & Levy, D. (1995). The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis and Rheumatism, 38(10), 1500–1505. https://doi.org/10.1002/art.1780381017
Funck‐Brentano, T., Nethander, M., Movérare‐Skrtic, S., Richette, P., & Ohlsson, C. (2019). Causal Factors for Knee, Hip, and Hand Osteoarthritis: A Mendelian Randomization Study in the UK Biobank. Arthritis & Rheumatology, 71(10), 1634–1641. https://doi.org/10.1002/art.40928
Georgiev, T., & Angelov, A. K. (2019). Modifiable risk factors in knee osteoarthritis: Treatment implications. Rheumatology International, 39(7), 1145–1157. https://doi.org/10.1007/s00296-019-04290-z
Gignac, M. A. M., Irvin, E., Cullen, K., Van Eerd, D., Beaton, D. E., Mahood, Q., McLeod, C., & Backman, C. L. (2020). Men and Women’s Occupational Activities and the Risk of Developing Osteoarthritis of the Knee, Hip, or Hands: A Systematic Review and Recommendations for Future Research. Arthritis Care & Research, 72(3), 378–396. https://doi.org/10.1002/acr.23855
Golightly, Y. M., Shiue, K. Y., Nocera, M., Guermazi, A., Cantrell, J., Renner, J. B., Padua, D. A., Cameron, K. L., Svoboda, S. J., Jordan, J. M., Loeser, R. F., Kraus, V. B., Lohmander, L. S., Beutler, A. I., & Marshall, S. W. (2023). Association of Traumatic Knee Injury With Radiographic Evidence of Knee Osteoarthritis in Military Officers. Arthritis Care & Research, 75(8), 1744–1751. https://doi.org/10.1002/acr.25072
Goulston, L., D’Angelo, S., Sanchez, M., Spector, T., Hart, D., & Arden, N. (2016). Is waist circumference a better predictor of incident symptomatic radiographic knee osteoarthritis, radiographic knee osteoarthritis and knee pain than body mass index over 10 years? Osteoarthritis and Cartilage, 24, S206–S207. https://doi.org/10.1016/j.joca.2016.01.402
Hammer, P. E., Shiri, R., Kryger, A. I., Kirkeskov, L., & Bonde, J. P. (2014). Associations of work activities requiring pinch or hand grip or exposure to hand-arm vibration with finger and wrist osteoarthritis: A meta-analysis. Scandinavian Journal of Work, Environment & Health, 40(2), 133–145. https://doi.org/10.5271/sjweh.3409
Hannan, M. T., Felson, D. T., Anderson, J. J., & Naimark, A. (1993). Habitual physical activity is not associated with knee osteoarthritis: The Framingham Study. The Journal of Rheumatology, 20(4), 704–709.
Harris, E. C., & Coggon, D. (2015). HIP osteoarthritis and work. Best Practice & Research Clinical Rheumatology, 29(3), 462–482. https://doi.org/10.1016/j.berh.2015.04.015
Harrison, T. R., & Fauci, A. S. (Eds.). (1998). Harrison’s principles of internal medicine (14th ed). McGraw-Hill, Health Professions Division.
Hart, D. J., & Spector, T. D. (1993). Cigarette smoking and risk of osteoarthritis in women in the general population: The Chingford study. Annals of the Rheumatic Diseases, 52(2), 93–96. https://doi.org/10.1136/ard.52.2.93
Hartnett, D. A., Milner, J. D., & DeFroda, S. F. (2023). Osteoarthritis in the Upper Extremity. The American Journal of Medicine, 136(5), 415–421. https://doi.org/10.1016/j.amjmed.2023.01.025
Hawker, G. A., Stewart, L., French, M. R., Cibere, J., Jordan, J. M., March, L., Suarez-Almazor, M., & Gooberman-Hill, R. (2008). Understanding the pain experience in hip and knee osteoarthritis—An OARSI/OMERACT initiative. Osteoarthritis and Cartilage, 16(4), 415–422. https://doi.org/10.1016/j.joca.2007.12.017
Herquelot, E., Bodin, J., Petit, A., Ha, C., Leclerc, A., Goldberg, M., Zins, M., Roquelaure, Y., & Descatha, A. (2015). Incidence of Chronic and Other Knee Pain in Relation to Occupational Risk Factors in a Large Working Population. Annals of Occupational Hygiene, 59(6), 797–811. https://doi.org/10.1093/annhyg/mev010
Higgins, D. M., Buta, E., Heapy, A. A., Driscoll, M. A., Kerns, R. D., Masheb, R., Becker, W. C., Hausmann, L. R. M., Bair, M. J., Wandner, L., Janke, E. A., Brandt, C. A., & Goulet, J. L. (2020). The Relationship Between Body Mass Index and Pain Intensity Among Veterans with Musculoskeletal Disorders: Findings from the MSD Cohort Study. Pain Medicine, 21(10), 2563–2572. https://doi.org/10.1093/pm/pnaa043
Hoffman, D. F. (1993). Arthritis and exercise. Primary Care, 20(4), 895–910.
Hulshof, C. T. J., Colosio, C., Daams, J. G., Ivanov, I. D., Prakash, K. C., Kuijer, P. P. F. M., Leppink, N., Mandic-Rajcevic, S., Masci, F., van der Molen, H. F., Neupane, S., Nygård, C.-H., Oakman, J., Pega, F., Proper, K., Prüss-Üstün, A. M., Ujita, Y., & Frings-Dresen, M. H. W. (2019). WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of exposure to occupational ergonomic risk factors and of the effect of exposure to occupational ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases. Environment International, 125, 554–566. https://doi.org/10.1016/j.envint.2018.09.053
Hulshof, C. T. J., Pega, F., Neupane, S., Colosio, C., Daams, J. G., Kc, P., Kuijer, P. P. F. M., Mandic-Rajcevic, S., Masci, F., van der Molen, H. F., Nygård, C.-H., Oakman, J., Proper, K. I., & Frings-Dresen, M. H. W. (2021). The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environment International, 150, 106349. https://doi.org/10.1016/j.envint.2020.106349
Janssen, I., & Mark, A. E. (2006). Separate and combined influence of body mass index and waist circumference on arthritis and knee osteoarthritis. International Journal of Obesity, 30(8), 1223–1228. https://doi.org/10.1038/sj.ijo.0803287
Johnson, V. L., & Hunter, D. J. (2014). The epidemiology of osteoarthritis. Best Practice & Research. Clinical Rheumatology, 28(1), 5–15. https://doi.org/10.1016/j.berh.2014.01.004
Kellgren, J. H., & Lawrence, J. S. (1952). Rheumatism in Miners. Part II: X-ray Study. Occupational and Environmental Medicine, 9(3), 197–207. https://doi.org/10.1136/oem.9.3.197
Kellgren, J. H., Lawrence, J. S., & Bier, F. (1963). Genetic Factors in Generalized Osteo-Arthrosis. Annals of the Rheumatic Diseases, 22(4), 237–255. https://doi.org/10.1136/ard.22.4.237
Kellgren, J. H., & Moore, R. (1952). Generalized osteoarthritis and Heberden’s nodes. British Medical Journal, 1(4751), 181–187. https://doi.org/10.1136/bmj.1.4751.181
Kelley, W. N., Harris, E., & Ruddy, S. (Eds.). (1993). Textbook of Rheumatology 4th Ed (4th ed, Vol. 2). Saunders.
Kelley, W. N., Harris, Ruddy, & Sledge. (1981). Textbook of Rheumatology 5th Ed: Vol. Vol. 2. (Issue v. 1-2). W.B. Saunders: Montreal. https://books.google.ca/books?id=Lp9LAQAAIAAJ
Kim, H. I., Ahn, S. H., Kim, Y., Lee, J. E., Choi, E., & Seo, S. K. (2022). Effects of sarcopenia and sarcopenic obesity on joint pain and degenerative osteoarthritis in postmenopausal women. Scientific Reports, 12(1), 13543. https://doi.org/10.1038/s41598-022-17451-1
Kim, S.-K., & Choe, J.-Y. (2022). Association between metabolic syndrome and radiographic spine osteoarthritis: Cross-sectional analysis using data from the Korea National Health and Nutrition Examination Survey. International Journal of Rheumatic Diseases, 25(4), 466–473. https://doi.org/10.1111/1756-185X.14296
Knapik, J. J., Pope, R., Orr, R., & Schram, B. (2018). Osteoarthritis: Pathophysiology, Prevalence, Risk Factors, and Exercise for Reducing Pain and Disability. Journal of Special Operations Medicine, 18(3), 94. https://doi.org/10.55460/V9VN-I71T
Kodama, R., Muraki, S., Oka, H., Iidaka, T., Teraguchi, M., Kagotani, R., Asai, Y., Yoshida, M., Morizaki, Y., Tanaka, S., Kawaguchi, H., Nakamura, K., Akune, T., & Yoshimura, N. (2016). Prevalence of hand osteoarthritis and its relationship to hand pain and grip strength in Japan: The third survey of the ROAD study. Modern Rheumatology, 26(5), 767–773. https://doi.org/10.3109/14397595.2015.1130673
Kujala, U. M., Kaprio, J., & Sarna, S. (1994). Osteoarthritis of weight bearing joints of lower limbs in former elite male athletes. BMJ (Clinical Research Ed.), 308(6923), 231–234. https://doi.org/10.1136/bmj.308.6923.231
Kulkarni, J., Adams, J., Thomas, E., & Silman, A. (1998). Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clinical Rehabilitation, 12(4), 348–353. https://doi.org/10.1191/026921598672393611
Kuş, G., Yasacı, Z., Boz, C., & Türkmen, E. (2023). Association of Osteoarthritis Prevalence With Age and Obesity Factors in Organization for Economic Cooperation and Development Countries: Panel Regression Model. American Journal of Physical Medicine & Rehabilitation, 102(10), 901–906. https://doi.org/10.1097/PHM.0000000000002244
Lane, N. E., Bloch, D. A., Jones, H. H., Marshall, W. H., Wood, P. D., & Fries, J. F. (1986). Long-distance running, bone density, and osteoarthritis. JAMA, 255(9), 1147–1151.
Lane, N. E., & Buckwalter, J. A. (1993). EXERCISE: A CAUSE OF OSTEOARTHRITIS? Rheumatic Disease Clinics of North America, 19(3), 617–633. https://doi.org/10.1016/S0889-857X(21)00335-5
Lawrence, J. S. (1969). Generalized osteoarthrosis in a population sample. American Journal of Epidemiology, 90(5), 381–389. https://doi.org/10.1093/oxfordjournals.aje.a121083
Lawrence, J. S., & Aitken-Swan, J. (1952). Rheumatism in Miners. Part I: Rheumatic Complaints. Occupational and Environmental Medicine, 9(1), 1–18. https://doi.org/10.1136/oem.9.1.1
Li, A. D.-F., Eccleston, C. T., Abraham, V., Balazs, G. C., & Goldman, A. H. (2022). Total hip and knee arthroplasty after lower extremity amputation in a military population. BMJ Military Health, e002106. https://doi.org/10.1136/military-2022-002106
Lo, G. H., Richard, M. J., McAlindon, T. E., Park, C., Strayhorn, M. T., Harkey, M. S., Price, L. L., Eaton, C. B., & Driban, J. B. (2022). Increased risk of incident knee osteoarthritis in those with greater work-related physical activity. Occupational and Environmental Medicine, 79(8), 543–549. https://doi.org/10.1136/oemed-2022-108212
Lovalekar, M., Hauret, K., Roy, T., Taylor, K., Blacker, S. D., Newman, P., Yanovich, R., Fleischmann, C., Nindl, B. C., Jones, B., & Canham-Chervak, M. (2021). Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. Journal of Science and Medicine in Sport, 24(10), 963–969. https://doi.org/10.1016/j.jsams.2021.03.016
Lundin, C. R., Houe, T., Sevelsted, A., & Nissen, L. (2016). Prolonged mounted patrolling is a risk factor for developing knee pain in Danish military personnel deployed to the Helmand Province. Journal of the Royal Army Medical Corps, 162(5), 348–351. https://doi.org/10.1136/jramc-2015-000511
MacCarty, D. J. (Ed.). (1989). Arthritis and allied conditions: A textbook of rheumatology (11th ed). Lea & Febiger.
McDaniel, W. J., & Dameron, T. B. (1983). The untreated anterior cruciate ligament rupture. Clinical Orthopaedics and Related Research, 172, 158–163.
McWilliams, D. F., Leeb, B. F., Muthuri, S. G., Doherty, M., & Zhang, W. (2011). Occupational risk factors for osteoarthritis of the knee: A meta-analysis. Osteoarthritis and Cartilage, 19(7), 829–839. https://doi.org/10.1016/j.joca.2011.02.016
Melcer, T., Walker, J., Sechriest, V. F., Bhatnagar, V., Richard, E., Perez, K., & Galarneau, M. (2019). A Retrospective Comparison of Five‐Year Health Outcomes Following Upper Limb Amputation and Serious Upper Limb Injury in the Iraq and Afghanistan Conflicts. PM&R, 11(6), 577–589. https://doi.org/10.1002/pmrj.12047
Migliorini, F., Maffulli, N., Pintore, A., Ernst, J., Eschweiler, J., Hildebrand, F., & Betsch, M. (2022). Osteoarthritis Risks and Sports: An Evidence-based Systematic Review. Sports Medicine and Arthroscopy Review, 30(3), 118–140. https://doi.org/10.1097/JSA.0000000000000351
National Collaborating Centre for Chronic Conditions (UK). (2008). Osteoarthritis: National Clinical Guideline for Care and Management in Adults. Royal College of Physicians (UK). http://www.ncbi.nlm.nih.gov/books/NBK48984/
Nedunchezhiyan, U., Varughese, I., Sun, A. R., Wu, X., Crawford, R., & Prasadam, I. (2022). Obesity, Inflammation, and Immune System in Osteoarthritis. Frontiers in Immunology, 13, 907750. https://doi.org/10.3389/fimmu.2022.907750
Osteoarthritis. (1994). Scientific American Medicine.
Orr, R., Schram, B., Canetti, E., & Pope, R. (2022). Exposure to risk factors for the development of lower limb osteoarthritis during Army infantry training. Journal of Science and Medicine in Sport, 25, S41. https://doi.org/10.1016/j.jsams.2022.09.032
O’Leary, T. J., Young, C. D., Wardle, S. L., & Greeves, J. P. (2023). Gender data gap in military research: A review of the participation of men and women in military musculoskeletal injury studies. BMJ Military Health, 169(1), 84–88. https://doi.org/10.1136/bmjmilitary-2021-002015
O’Sullivan, O., Behan, F. P., Coppack, R. J., Stocks, J., Kluzek, S., Valdes, A. M., & Bennett, A. N. (2023). Osteoarthritis in the UK Armed Forces: A review of its impact, treatment and future research. BMJ Military Health, e002390. https://doi.org/10.1136/military-2023-002390
Palmer, D., Cooper, D., Whittaker, J. L., Emery, C., Batt, M. E., Engebretsen, L., Schamasch, P., Shroff, M., Soligard, T., Steffen, K., & Budgett, R. (2022). Prevalence of and factors associated with osteoarthritis and pain in retired Olympians compared with the general population: Part 2 – the spine and upper limb. British Journal of Sports Medicine, 56(19), 1132–1141. https://doi.org/10.1136/bjsports-2021-104978
Palmer, K. T. (2012). Occupational activities and osteoarthritis of the knee. British Medical Bulletin, 102(1), 147–170. https://doi.org/10.1093/bmb/lds012
Panush, R. S., & Brown, D. G. (1987). Exercise and arthritis. Sports Medicine (Auckland, N.Z.), 4(1), 54–64. https://doi.org/10.2165/00007256-198704010-00006
Park, D., Park, Y.-M., Ko, S.-H., Hyun, K.-S., Choi, Y.-H., Min, D.-U., Han, K., & Koh, H.-S. (2023). Association of general and central obesity, and their changes with risk of knee osteoarthritis: A nationwide population-based cohort study. Scientific Reports, 13(1), 3796. https://doi.org/10.1038/s41598-023-30727-4
Perry, T. A., Wang, X., Gates, L., Parsons, C. M., Sanchez-Santos, M. T., Garriga, C., Cooper, C., Nevitt, M. C., Hunter, D. J., & Arden, N. K. (2020). Occupation and risk of knee osteoarthritis and knee replacement: A longitudinal, multiple-cohort study. Seminars in Arthritis and Rheumatism, 50(5), 1006–1014. https://doi.org/10.1016/j.semarthrit.2020.08.003
Plotz, B., Bomfim, F., Sohail, M. A., & Samuels, J. (2021). Current Epidemiology and Risk Factors for the Development of Hand Osteoarthritis. Current Rheumatology Reports, 23(8), 61. https://doi.org/10.1007/s11926-021-01025-7
Reyes, C., Leyland, K. M., Peat, G., Cooper, C., Arden, N. K., & Prieto‐Alhambra, D. (2016). Association Between Overweight and Obesity and Risk of Clinically Diagnosed Knee, Hip, and Hand Osteoarthritis: A Population‐Based Cohort Study. Arthritis & Rheumatology, 68(8), 1869–1875. https://doi.org/10.1002/art.39707
Rhon, D. I., Molloy, J. M., Monnier, A., Hando, B. R., & Newman, P. M. (2022). Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta‐analysis. European Journal of Sport Science, 22(1), 16–34. https://doi.org/10.1080/17461391.2021.1931464
Rhon, D. I., Perez, K. G., & Eskridge, S. L. (2019). Risk of post‐traumatic knee osteoarthritis after knee injury in military service members. Musculoskeletal Care, 17(1), 113–119. https://doi.org/10.1002/msc.1378
Rhon, D. I., Teyhen, D. S., Kiesel, K., Shaffer, S. W., Goffar, S. L., Greenlee, T. A., & Plisky, P. J. (2022). Recovery, Rehabilitation, and Return to Full Duty in a Military Population After a Recent Injury: Differences Between Lower-Extremity and Spine Injuries. Arthroscopy, Sports Medicine, and Rehabilitation, 4(1), e17–e27. https://doi.org/10.1016/j.asmr.2021.09.028
Rivera, J. C., Wenke, J. C., Buckwalter, J. A., Ficke, J. R., & Johnson, A. E. (2012). Posttraumatic Osteoarthritis Caused by Battlefield Injuries: The Primary Source of Disability in Warriors. Journal of the American Academy of Orthopaedic Surgeons, 20, S64–S69. https://doi.org/10.5435/JAAOS-20-08-S64
Robinson, D. (n.d.). Osteoarthritis. Scientific American Journal.
Rodriguez, M. J., Garcia, E. J., & Dickens, J. F. (2019). Primary and Posttraumatic Knee Osteoarthritis in the Military. The Journal of Knee Surgery, 32(2), 134–137. https://doi.org/10.1055/s-0038-1676956
Rossignol, M. (2005). Primary osteoarthritis of hip, knee, and hand in relation to occupational exposure. Occupational and Environmental Medicine, 62(11), 772–777. https://doi.org/10.1136/oem.2005.020057
Rubak, T. S., Svendsen, S. W., Andersen, J. H., Haahr, J. P. L., Kryger, A., Jensen, L. D., & Frost, P. (2014). An expert-based job exposure matrix for large scale epidemiologic studies of primary hip and knee osteoarthritis: The Lower Body JEM. BMC Musculoskeletal Disorders, 15(1), 204. https://doi.org/10.1186/1471-2474-15-204
Rudzki, with S., Delaney, T., & Macri, E. (2017). Military personnel. In P. Brukner, B. Clarsen, J. Cook, A. Cools, K. Crossley, M. Hutchinson, P. McCrory, R. Bahr, & K. Khan (Eds.), Brukner & Khan’s Clinical Sports Medicine: Injuries, Volume 1, 5e (1–Book, Section). McGraw-Hill Education. https://csm.mhmedical.com/content.aspx?bookid=1970§ionid=168697060
Sakellariou, G., Conaghan, P. G., Zhang, W., Bijlsma, J. W. J., Boyesen, P., D’Agostino, M. A., Doherty, M., Fodor, D., Kloppenburg, M., Miese, F., Naredo, E., Porcheret, M., & Iagnocco, A. (2017). EULAR recommendations for the use of imaging in the clinical management of peripheral joint osteoarthritis. Annals of the Rheumatic Diseases, 76(9), 1484–1494. https://doi.org/10.1136/annrheumdis-2016-210815
Samanta, A., Jones, A., Regan, M., Wilson, S., & Doherty, M. (1993). Is osteoarthritis in women affected by hormonal changes or smoking? British Journal of Rheumatology, 32(5), 366–370. https://doi.org/10.1093/rheumatology/32.5.366
Sammito, S., Hadzic, V., Karakolis, T., Kelly, K. R., Proctor, S. P., Stepens, A., White, G., & Zimmermann, W. O. (2021). Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Military Medical Research, 8(1), 66. https://doi.org/10.1186/s40779-021-00357-w
Sampath, S. J. P., Venkatesan, V., Ghosh, S., & Kotikalapudi, N. (2023). Obesity, Metabolic Syndrome, and Osteoarthritis—An Updated Review. Current Obesity Reports, 12(3), 308–331. https://doi.org/10.1007/s13679-023-00520-5<
Saville, P. D., & Dickson, J. (1968). Age and weight in osteoarthritis of the hip. Arthritis & Rheumatism, 11(5), 635–644. https://doi.org/10.1002/art.1780110505
Schram, B., Orr, R., Pope, R., Canetti, E., & Knapik, J. (2020). Risk factors for development of lower limb osteoarthritis in physically demanding occupations: A narrative umbrella review. Journal of Occupational Health, 62(1), e12103. https://doi.org/10.1002/1348-9585.12103
Sergent, J. S. (1993). Polyarticular Arthritis in Kelley’s Textbook of Rheumatology: Vol. Volume 2 (E. D. Harris, S. Ruddy, & C. B. Sledge, Eds.; Fourth Edition).
Shumnalieva, R., Kotov, G., & Monov, S. (2023). Obesity-Related Knee Osteoarthritis—Current Concepts. Life, 13(8), 1650. https://doi.org/10.3390/life13081650
Sim, B., Lee, J., Lee, C. G., & Song, H. (2022). Radiographic hand osteoarthritis in women farmers: Characteristics and risk factors. Annals of Occupational and Environmental Medicine, 34(1), e10. https://doi.org/10.35371/aoem.2022.34.e10
Simas, V., Orr, R., Schram, B., Canetti, E., Campbell, P., & Pope, R. (2022). Occupational factors associated with the development of spondylosis in physically demanding occupations: A rapid review. Journal of Science and Medicine in Sport, 25, S10–S11. https://doi.org/10.1016/j.jsams.2022.09.132
Spahn, G., Lipfert, J. U., Maurer, C., Hartmann, B., Schiele, R., Klemm, H.-T., Grifka, J., & Hofmann, G. O. (2017). Risk factors for cartilage damage and osteoarthritis of the elbow joint: Case-control study and systematic literature review. Archives of Orthopaedic and Trauma Surgery, 137(4), 557–566. https://doi.org/10.1007/s00402-017-2654-6
Srikanth, V. K., Fryer, J. L., Zhai, G., Winzenberg, T. M., Hosmer, D., & Jones, G. (2005). A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis and Cartilage, 13(9), 769–781. https://doi.org/10.1016/j.joca.2005.04.014
Steelman, T., Lewandowski, L., Helgeson, M., Wilson, K., Olsen, C., & Gwinn, D. (2018). Population-based Risk Factors for the Development of Degenerative Disk Disease. Clinical Spine Surgery: A Spine Publication, 31(8), E409–E412. https://doi.org/10.1097/BSD.0000000000000682
Struyf, P. A., van Heugten, C. M., Hitters, M. W., & Smeets, R. J. (2009). The Prevalence of Osteoarthritis of the Intact Hip and Knee Among Traumatic Leg Amputees. Archives of Physical Medicine and Rehabilitation, 90(3), 440–446. https://doi.org/10.1016/j.apmr.2008.08.220
Sun, Y., Nold, A., Glitsch, U., & Bochmann, F. (2019). Exposure–Response Relationship and Doubling Risk Doses—A Systematic Review of Occupational Workload and Osteoarthritis of the Hip. International Journal of Environmental Research and Public Health, 16(19), 3681. https://doi.org/10.3390/ijerph16193681
Teichtahl, A. J., Smith, S., Wang, Y., Wluka, A. E., O’Sullivan, R., Giles, G. G., & Cicuttini, F. M. (2015). Occupational risk factors for hip osteoarthritis are associated with early hip structural abnormalities: A 3.0 T magnetic resonance imaging study of community-based adults. Arthritis Research & Therapy, 17(1), 19. https://doi.org/10.1186/s13075-015-0535-3
Textbook of rheumatology (4th ed). (1993). W. B. Saunders.
van Saase, J. L., van Romunde, L. K., Cats, A., Vandenbroucke, J. P., & Valkenburg, H. A. (1989). Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Annals of the Rheumatic Diseases, 48(4), 271–280. https://doi.org/10.1136/ard.48.4.271
Venn, A. J., & Guest, C. S. (1991). Chronic morbidity of former prisoners of war and other Australian veterans. The Medical Journal of Australia, 155(10), 705–707, 710–712.
Veterans Affairs Canada (2024). Knee Joint Osteoarthritis. License purchased for use from Knee Osteoarthritis And Normal Joint Detailed Anatomy Royalty Free SVG, Cliparts, Vectors, and Stock Illustration. Image 39337948. (123rf.com)
Veterans Affairs Canada (2024). Hip Joint Osteoarthritis. License purchased for use from Arthritis Of The Hip Joint, Healthy Joint And Unhealthy Joint With Damaged Cartilage And Osteophytes. Royalty Free SVG, Cliparts, Vectors, and Stock Illustration. Image 40404431. (123rf.com)
Vingård, E., Alfredsson, L., Goldie, I., & Hogstedt, C. (1991). Occupation and osteoarthrosis of the hip and knee: A register-based cohort study. International Journal of Epidemiology, 20(4), 1025–1031. https://doi.org/10.1093/ije/20.4.1025
Wang, T., & He, C. (2018). Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine & Growth Factor Reviews, 44, 38–50. https://doi.org/10.1016/j.cytogfr.2018.10.002
Wasser, J. G., Hendershot, B. D., Acasio, J. C., Krupenevich, R. L., Pruziner, A. L., Miller, R. H., Goldman, S. M., Valerio, M. S., Senchak, L. T., Murphey, M. D., Heltzel, D. A., Fazio, M. G., Dearth, C. L., & Hager, N. A. (2024). A Comprehensive, Multidisciplinary Assessment for Knee Osteoarthritis Following Traumatic Unilateral Lower Limb Loss in Service Members. Military Medicine, 189(3–4), 581–591. https://doi.org/10.1093/milmed/usac203
Welke, B., Jakubowitz, E., Seehaus, F., Daniilidis, K., Timpner, M., Tremer, N., Hurschler, C., & Schwarze, M. (2019). The prevalence of osteoarthritis: Higher risk after transfemoral amputation?—A database analysis with 1,569 amputees and matched controls. PLOS ONE, 14(1), e0210868. https://doi.org/10.1371/journal.pone.0210868
Wijnhoven, H. A. H., de Vet, H. C. W., & Picavet, H. S. J. (2006). Prevalence of Musculoskeletal Disorders Is Systematically Higher in Women Than in Men. The Clinical Journal of Pain, 22(8), 717–724. https://doi.org/10.1097/01.ajp.0000210912.95664.53
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/
Yavnai, N., Bar-Sela, S., Pantanowitz, M., Funk, S., Waddington, G., Simchas, L., Svorai-Litvak, S., & Steinberg, N. (2021). Incidence of injuries and factors related to injuries in combat soldiers. BMJ Military Health, 167(6), 418–423. https://doi.org/10.1136/jramc-2019-001312
Zhang, W., Doherty, M., Leeb, B. F., Alekseeva, L., Arden, N. K., Bijlsma, J. W., Dincer, F., Dziedzic, K., Hauselmann, H. J., Kaklamanis, P., Kloppenburg, M., Lohmander, L. S., Maheu, E., Martin-Mola, E., Pavelka, K., Punzi, L., Reiter, S., Smolen, J., Verbruggen, G., … Zimmermann-Gorska, I. (2009). EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: Report of a task force of ESCISIT. Annals of the Rheumatic Diseases, 68(1), 8–17. https://doi.org/10.1136/ard.2007.084772